With 40,000 people being diagnosed with type 1 diabetes every year in the U.S. alone, separating the myths from the facts is the first step to taking control of the lifelong disorder. And with so many people living with this condition, it’s important we provide the best information, not only for them, but also their friends and family.
The Cause is Relatively Unknown
There is currently no cure for type 1 diabetes and it’s not entirely understood why it occurs. However, according to Mayo Clinic and EndoctrineWeb, some known risk factors for type 1 diabetes include:
- Family history: Anyone with a parent or sibling with type 1 diabetes has a slightly increased risk of developing the condition. This risk is higher when the father has type 1 diabetes, and even higher when both parents have type 1 diabetes.
- Genetics: The presence of a certain genetic marker indicates an increased risk of developing type 1 diabetes. That genetic marker is located on chromosome 6, and it’s an HLA (human leukocyte antigen) complex.
- Viral infections: Certain viruses may trigger the development of type 1 diabetes by causing the immune system to turn against the body—instead of helping it fight infection and sickness. Viruses that are believed to trigger type 1 include German measles, coxsackie, and mumps.
- Age: Although type 1 diabetes can appear at any age, it appears at two noticeable peaks. The first peak occurs in children between 4- and 7-years-old, and the second is in children between 10 and 14-years-old.
Symptoms Can be Difficult to Distinguish From Other Medical Conditions
Symptoms can show very early on in people with type diabetes; over the course of only weeks or months after its onset. However, type 1 diabetes shares many symptoms with other conditions and disorders, making it hard to personally diagnose. This is why it’s important to take notice of any changes in your body and get checked by your doctor at the first sign of anything that could even remotely be related to type 1 diabetes.
Symptoms Associated with Type 1 Diabetes
- Excessive urination or bed-wetting in children (the result of your kidneys trying to expel excess sugar in your blood)
- Feeling very thirsty, experiencing a dry mouth, or having itchy skin (due to the dehydration caused by your kidneys trying to expel excess sugar in your blood)
- Feeling very tired or weak, increased hunger (especially after eating), unintended weight loss, or loss of muscle bulk (due to your body not getting adequate energy from the food you eat)
- Frequent or recurring infections, slow-healing cuts or bruises, tingling or numbness in the hands or feet, or difficulty getting or maintaining erections in men (due to high blood sugar levels affecting blood flow and causing nerve damage, which in turn makes healing difficult)
- Frequent yeast infections (due to yeast infections feeding on glucose)
- Blurred vision (due to the lens of your eye changing shape)
Complications of Type 1 Diabetes
Not seeking medical attention can lead to more severe complications. These complications can be both short- and long-term and can affect your nerves, heart, blood vessels, eyes, and kidney.
If untreated or mistreated, complications that can arise from type 1 diabetes include:
- Hypoglycemia (low blood sugar)
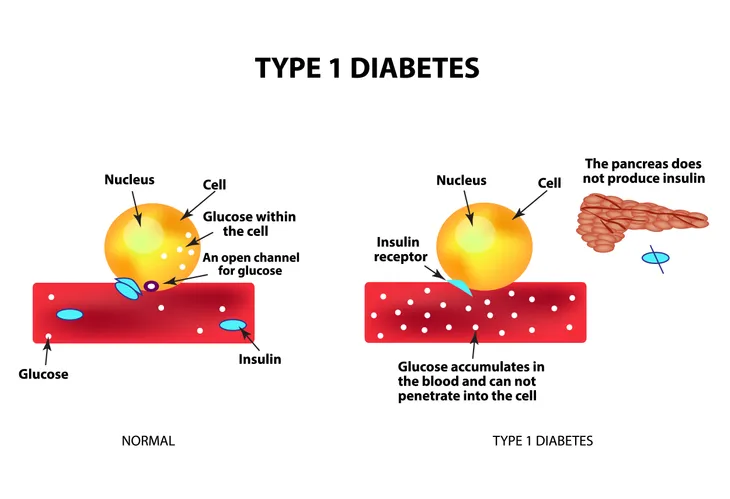
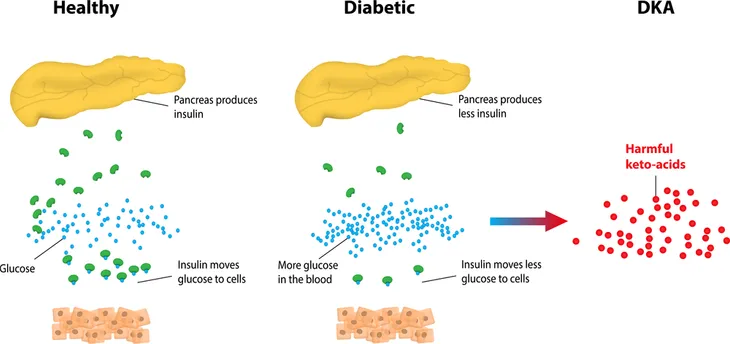
- Diabetic Ketoacidosis (acid buildup in your blood)
- Cataracts and/or retinopathy in your eyes
- Kidney failure
- Nerve damage (most commonly affecting the feet)
- Coronary artery disease
- Heart attack
- Stroke
- Atherosclerosis (narrowing of the arteries)
- High blood pressure
More Than One Way to Administer Treatment for Type 1 Diabetes
Hormone treatment is the only way to treat type 1 diabetes, but there’s more than one way to administer it. You can manually inject, which is the most common form. This requires multiple daily injections that include a combination of a long-acting and rapid-acting to try to mimic the body’s normal use of the hormone. The number of shots required each day will be different from person to person and can change depending on the state of your diabetes (as overseen by your doctor).
Another option is the pump, which consists of a device that you have to wear on the outside of your body with a tube that inserts under the skin of your stomach. A physician or health care professional programs the pump to determine how much of the hormone that allows glucose to be used as energy to give. Based on the meals you eat and your blood sugar levels throughout the day, this tube then automatically administers specific amounts of the rapid-acting form of the hormone.
For those interested, the hormone that regulates glucose in your blood can’t be taken orally. If taken orally, the hormone would break down in your intestines before it’s able to have any medicinal effect.
Both of these methods require you to prick your finger to get a read on your blood glucose levels. If you want to avoid constant pricking, you can use continuous glucose monitoring (CGM). Worn for one to two weeks at a time, this device features a tiny sensor — implanted under the skin — that senses blood sugar levels every 5 minutes. However, CGM is not yet considered to be as accurate as standard blood sugar monitoring, so checking your blood sugar levels manually is still recommended.
Treating and Managing Type 1 Diabetes is a Lifestyle
Type 1 diabetes requires a holistic approach to treatment consisting of blood glucose monitoring, hormone dosing, routine checkups, a healthy diet, and exercise.
Blood Glucose Monitoring and Hormone Dosing
To give you an idea of how unpredictable your blood glucose levels can be, consider all the different factors that can affect blood sugar levels:
- Food
- Stress
- Hormone changes
- Periods of growth
- Illness
- Physical activity
Even when following a strict meal and dosing schedule, any one or combination of things above can result in blood sugar levels fluctuating unpredictably.
To illustrate how all of these different factors can affect one another, starting a new exercise regime and exerting more physical effort than normal will likely require you, as overseen by your doctor, to alter your dosing amount and meal plan. This is because physical activity causes blood glucose levels to drop, which requires you to eat something sugary to bring those levels back up, which requires a hormone dose for your body to be able to effectively use that glucose.
While this is completely natural, it also explains why constant monitoring is so important, regardless of how familiar someone is with what they’re eating or what they’re doing.
Although your doctor will recommend a monitoring schedule, the American Diabetes Association recommends testing blood sugar levels before meals and snacks, before bed, before exercising or driving, and any time you suspect you may have low blood sugar.