Multiple sclerosis (MS) is a neurologic condition that has many similarities to other medical conditions. Unfortunately, there is no single diagnostic tool used to determine if someone has multiple sclerosis, making misdiagnoses more common than most people think. In fact, according to an article from the journal of Multiple Sclerosis and Related Disorders, 18-percent of new multiple sclerosis patients were initially diagnosed with a different condition.
Here we cover many of the conditions that are commonly mistaken for multiple sclerosis. These conditions share some of the same symptoms or similar causes to multiple sclerosis. However, with each condition, you’ll see their differences from multiple sclerosis.
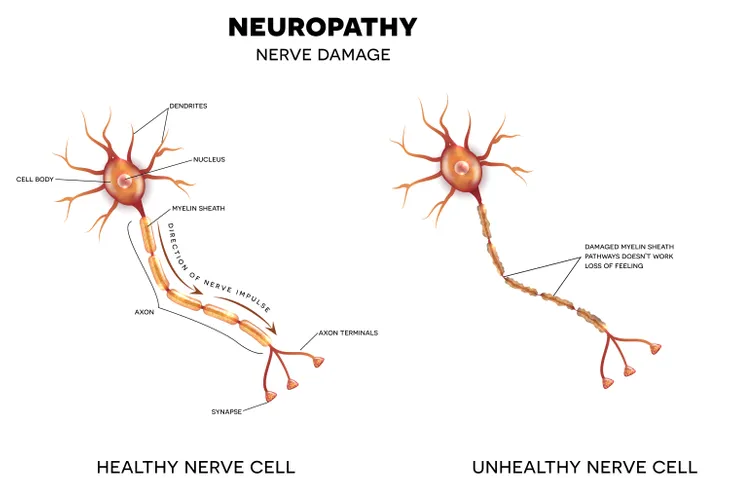
1. Neuropathy
Neuropathy, sometimes called peripheral neuropathy, is a condition when the nervous system is damaged somewhere outside of the brain and spinal cord. People who suffer from this condition may feel a pins and needles sensation, pain, numbness, and weakness. Neuropathy is more common in people with diabetes because high blood sugar levels can damage the peripheral nerves.
Multiple sclerosis and neuropathy share some of the same symptoms making it difficult to get the right diagnosis. However, neuropathy is unique in that it has different subsets of the condition: sensory, motor, and autonomic. With each one of those subsets having, “their own set of symptoms, many of which differ from the common symptoms of MS” reports Everyday Health.
2. Brain Tumor
Another condition that can be mistaken for multiple sclerosis is a brain tumor says the National Multiple Sclerosis Society. Brain tumors can cause a multitude of effects on the body ranging from numbness and tingling to vision changes and loss of balance. Because of the wide range of symptoms caused by brain tumors, it can be hard for physicians to determine exactly what’s causing the symptoms.
Anyone with these symptoms will likely need to have an MRI for a diagnosis. MRIs are one of the many diagnostic tools used to diagnose both brain tumors and multiple sclerosis. On top of that, tumors can spread to other parts of the body causing other symptoms not associated with MS.
3. Radiologically Isolated Syndrome
MRIs can show so many different changes within your brain, one of which is radiologically isolated syndrome. People with this syndrome don’t have symptoms of multiple sclerosis but they do have the characteristic brain lesions like someone with MS. Not everyone with radiologically isolated syndrome will go on to develop multiple sclerosis, but some will states the MS International Federation.
Radiologically isolated syndrome may be an early indicator of multiple sclerosis. And because of its similar presentation to MS on an MRI, it can be misdiagnosed. Everyday Health reported a study from the Multiple Sclerosis and Related Disorders Journal, “up to 10-percent of people misdiagnosed with — and being treated for — MS in fact had radiologically isolated syndrome.” That’s a staggering number of people who don’t have the clinical symptoms of MS but are treated as such.
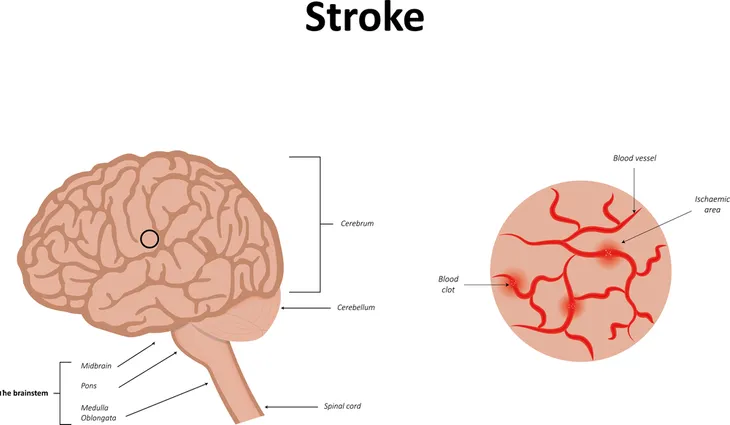
4. Stroke
A stroke is a serious medical condition where a vessel in your brain is blocked or breaks open. The blockage or rupture causes a lack of blood to flow to part of the brain. Without adequate blood flow, the brain doesn’t receive the oxygen and nutrients it needs. The symptoms of a stroke can include difficulty speaking, unsteady walking, vision changes, and much more.
Multiple sclerosis can have similar symptoms. However, the typical distinguishing features of a stroke is the person’s age and the onset of the symptoms. “While MS can occur in 70-year-olds, if the person is older, you tend to think of stroke, not MS,” says Everyday Health. A stroke is a medical emergency, don’t delay seeking treatment if you or someone you know is having a stroke.
5. Lyme Disease
Lyme disease is carried by ticks and can be transmitted to humans through a tick bite. The bacterial infection, “affects the nervous system in about 10- to 15-percent of people infected with it,” reports VeryWell Health. The brain MRI of someone with Lyme disease can have similar findings as that of someone with multiple sclerosis. The clinical symptoms of late Lyme disease are similar to multiple sclerosis symptoms making a differential diagnosis difficult.
Do your research to find out if you live in an area that has ticks with Lyme disease. If you find a tick on your body remove it with a fine tipped tweezers, making sure to get the entire body and head. According to the CDC, place the tick in a sealed bag or container to bring it to your doctor for identification. Your doctor may prescribe a one time dose of antibiotics if he or she believes you are at risk for Lyme disease.
6. Lupus
Lupus is an autoimmune disease that mimics many of the symptoms of multiple sclerosis. Muscle pain, fatigue, headaches, and joint swelling are just a few of the symptoms those with lupus may have. One of the tell-tale signs of lupus that about half of those diagnosed will develop is a butterfly shaped rash over the cheeks and nose.
Since the symptoms are similar to so many other conditions, a lupus diagnosis will require multiple tests done by a specialist. Misdiagnosing multiple sclerosis for lupus can cause patients to receive unnecessary treatment and incur unneeded costs.
7. Migraine
If you’ve had a migraine you’re familiar with the incredible pain, sensitivity to light, nausea, and blurred vision they can produce. Migraines can occur in those with multiple sclerosis making them difficult to diagnose correctly. A study described by Everyday Health, “found that migraine was the most common correct diagnosis in study subjects who had been misdiagnosed with MS, occurring in 16-percent of them.”
Physicians use some of the same methods to diagnose migraines as they do to diagnose multiple sclerosis. Expect your doctor to ask you about your health history and perform a neurological exam. It’s important to be prepared with questions when visiting your doctor to make sure you get the best care possible and a fast diagnosis.
8. Conversion Disorder
Conversion disorder is a physical manifestation of psychological distress. People have experienced numbness, blindness, and paralysis that have no medical explanation. The symptoms typically start after a stressful event and are more common in people with personality disorders, dissociative disorder, or a medical illness reports Medline Plus.
This condition can be mistaken for multiple sclerosis. Everyday Health details that the journal, Neurology, published that, “11-percent of subjects definitely or probably misdiagnosed with MS actually had a conversion or psychogenic disorder.” That is a significant percentage of people who were mistakenly diagnosed and did not receive the correct treatment they needed.
9. Spondylopathy
Spondylopathy is a broad term for a disease or disorder that involves the spinal vertebrae. One type of spondylopathy, cervical spondylosis, can create traits similar to multiple sclerosis. According to the National MS Society, cervical spondylosis is, “a degeneration of the spine associated with normal aging that can press on the spinal cord and cause neurologic symptoms.”
Patients with spondylopathies were misdiagnosed with multiple sclerosis as much as 7-percent according to a study reported by Everyday Health. With so many overlapping symptoms, tingling, numbness, and limb weakness, it’s easy to see how these two conditions can be mistaken for each other. With a thorough health exam and testing, a doctor will be able to uncover the uniqueness of each disease and determine exactly the cause of your symptoms.
10. Neuromyelitis Optica
This inflammatory disease breaks down the myelin sheath that covers nerve fibers, similar to multiple sclerosis. The break down occurs on the optic nerves and spinal cord causing visual changes states the National Multiple Sclerosis Society. A differentiation between MS and neuromyelitis optica (NMO) is that in the early stages of NMO the brain is not affected.
Finding out exactly what’s causing the changes in eyesight can be a daunting task, yet incredibly critical. Everyday Health reports that, “treatments for MS are ineffective for and can even worsen NMOSD, so getting an accurate diagnosis is extremely important. A blood test known as the NMO IgG antibody test can help to differentiate between MS and NMOSD.”
11. Fibromyalgia
Fibromyalgia is a chronic condition characterized by pain, tiredness, mind fog, and mood changes. The widespread pain and other symptoms cannot be attributed to a specific source, which is one of the main features of fibromyalgia. With multiple sclerosis, sufferers will also have similar symptoms but specific testing should find the results leading to a MS diagnosis.
There isn’t one test used to diagnose MS. An MRI can find lesions on the brain and spinal cord. A doctor can perform a lumbar puncture, or spinal tap, to get cerebral spinal fluid (CSF) to test for antibodies typically found in people with MS. Both conditions require a comprehensive screening to help the patient get the correct diagnosis.
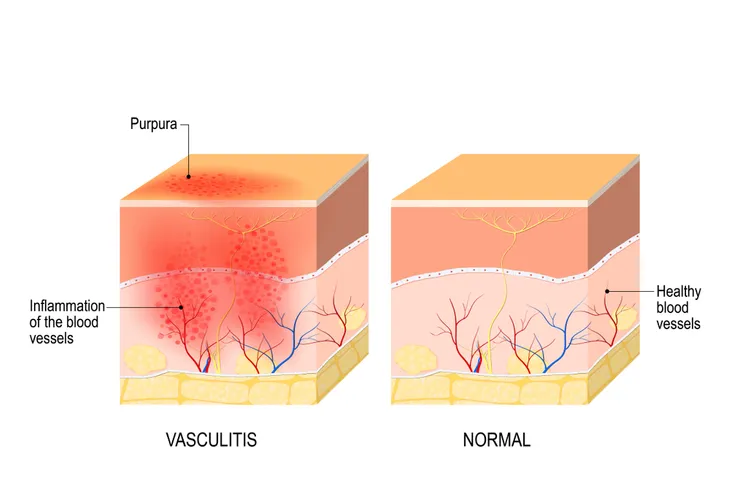
12. Vasculitis
Vasculitis is when the blood vessels become inflamed causing less blood to be able to pass through the vessels. If the inflammation becomes severe enough the vessels can cut off blood flow to areas of the body causing further damage. Symptoms associated with vasculitis are dependent on the location but can include pain, tingling, and fever.
With such generalized symptoms, it can be hard to distinguish the specific cause. This makes vasculitis a condition that can be mistaken for multiple sclerosis. If your doctor is suspecting vasculitis there are specific tests associated with the condition that can help form the differential diagnosis.
13. B12 Deficiency
Something as simple as a B12 deficiency can mimic the symptoms of multiple sclerosis. In B12 vitamin deficiency, “the myelin sheath surrounding nerve fibers is not formed properly, which impairs nerve signaling. This may cause MS-like symptoms, such as weakness, problems walking, cognitive dysfunction, and sensory disturbances like Lhermitte’ sign” says VeryWell Health.
Though the symptoms are similar, the conditions are very different. Multiple sclerosis affects the central nervous system, which includes the brain and spinal cord. A B12 deficiency affects the peripheral nervous system, which includes the nerves in the arms and legs. You can correct a B12 deficiency with diet changes or supplements. Whereas, multiple sclerosis is a chronic disease that has treatments but no cure.
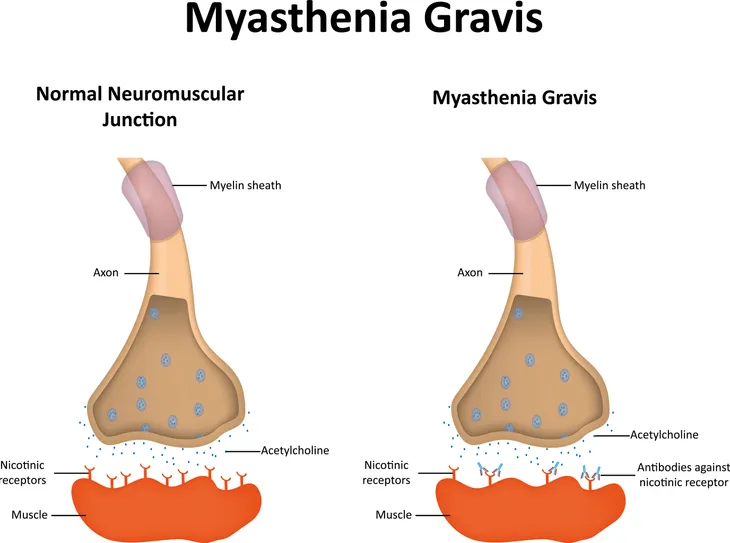
14. Myasthenia Gravis
Like multiple sclerosis, myasthenia gravis is a chronic autoimmune disease. Some of its initial symptoms are drooping eyelids and double vision. The disease progresses to muscle weakness that happens because of, “a defect in the transmission of nerve impulses to muscles” reports Everyday Health.
Myasthenia gravis is a condition that has many similarities to multiple sclerosis, yet its differences are what sets it apart. Muscle weakness can come and go, usually better after rest and worse when the muscles are being used. Your doctor can perform testing to determine if you or a loved one has this condition.
15. Acute Disseminated Encephalomyelitis
Acute disseminated encephalomyelitis (ADEM) is a serious inflammatory response that affects the central nervous system, which includes the spinal cord and brain. Since multiple sclerosis also affects the central nervous system these two conditions share many of the same symptoms like difficulty walking, fatigue, and vision loss.
However, with ADEM the cause is a viral or bacterial infection, so sufferers will also have fever and vomiting. Everyday Health says, “children are more likely to have ADEM, while MS is more likely to occur in adults.” With these significant differences, your doctor should be able to determine the cause of your symptoms with a detailed health history and testing.
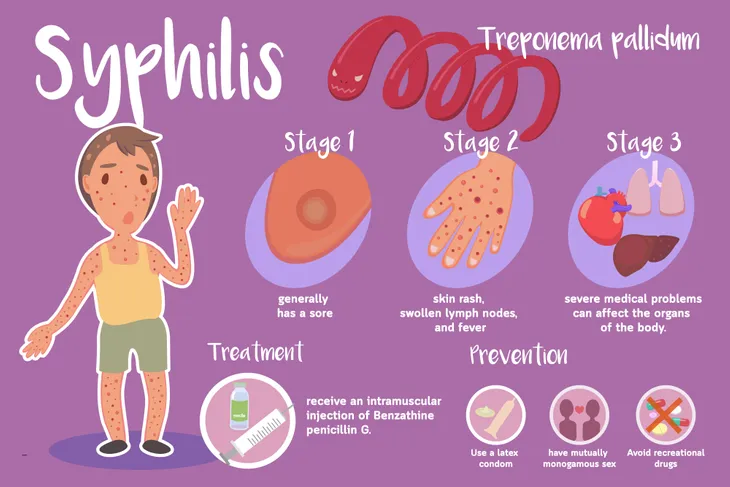
16. Syphilis
Though incredibly different conditions, syphilis and multiple sclerosis, can be mistaken for each other based on the similarities of their neurological symptoms. Syphilis is a sexually transmitted disease that can cause, “memory problems, slurred speech, tremor, sensory disturbances, and difficulties walking” details Everyday Health.
Unlike multiple sclerosis, syphilis can be diagnosed with a blood test and has a successful treatment plan if caught early. Once diagnosed, a doctor can prescribe an antibiotic to treat and cure syphilis.
17. Sarcoidosis
Sarcoidosis is a rare condition that causes clumps of inflammatory cells to grow in different areas of the body. The groupings of cells typically occur on the skin, eyes, lymph nodes, and lungs. It can go away on its own without treatment or can last for years. The symptoms are dependent on the location of the growths but can include difficulty breathing, fatigue, pain, swelling, and swollen lymph nodes.
Because sarcoidosis is caused by an overactive immune system it can be mistaken for multiple sclerosis. A sarcoidosis diagnosis can be difficult to make because of its generalized symptoms. Mayo Clinic says that a doctor may perform biopsies to look at the affected tissue or perform other testing to rule out other conditions.
18. Behcet’s Disease
Another autoimmune disease that can be mistaken for multiple sclerosis is Behcet’s disease. This condition causes inflammation in the blood vessels throughout the body. The symptoms can range from mouth sores to inflammation in the brain says the Mayo Clinic.
Because Behcet’s disease can produce such a wide range of symptoms that seemingly have little in common it can be difficult to diagnose. When the symptoms start to include neurologic signs then you can understand why multiple sclerosis can be mistaken for this condition.