Neuromyelitis optica (NMO) and multiple sclerosis (MS) are often confused with each other because they share some similarities, but they are definitely two completely separate conditions with major differences. One thing they do share in common is that, unfortunately, both NMO and MS are fairly common, particularly in North America. According to the National Multiple Sclerosis Society, NMO affects an estimated 4,000 people in the U.S. and a 250,000 people worldwide. On the other hand, nearly 1-million people in the U.S. are living with MS and an average of 1 in every 385 Canadians.
Due to the prevalence of both NMO and MS, as well as the misunderstanding around both of them, it’s important we take some time to learn more about these conditions. To get better informed, take some time to read this article which will provide an explanation of each condition, point out their similarities, and finally outline some of the major differences. Take a look…
What is Neuromyelitis Optica?
Sometimes referred to as Devic’s disease, NMO is an autoimmune disorder that causes the cells and antibodies in the immune system to attack the optic nerves and spinal cord. It can even cause them to attack the brain. Not surprisingly, these attacks can cause some serious damage starting with swelling and inflammation, which can lead to pain and loss of vision. The damage to the spinal cord results in weakness or paralysis in the legs or arms, loss of sensation, and problems with the bladder and bowel function, says the National Multiple Sclerosis Society.
The source goes on to explain that NMO is a relapsing-remitting disease, which means it comes and goes. As a result, the condition can get worse over time with every new relapse as new damage to the optic nerves and/or spinal cord leads to accumulating disability. Another important thing to know is that the cause of NMO is largely unknown, but it’s thought to be “due to a specific attack on the aquaporin-4 (AQP4) water channel located within the optic nerves and spinal cord,” writes the National Multiple Sclerosis Society. “Aquaporins (AQPs) are proteins that transport water across cell membranes.” More than 70-percent of NMO and NMOSD patients test positive for an antibody marker in their blood. These markers are either NMO-IgG or anti-AQP4 antibody.
What is Multiple Sclerosis?
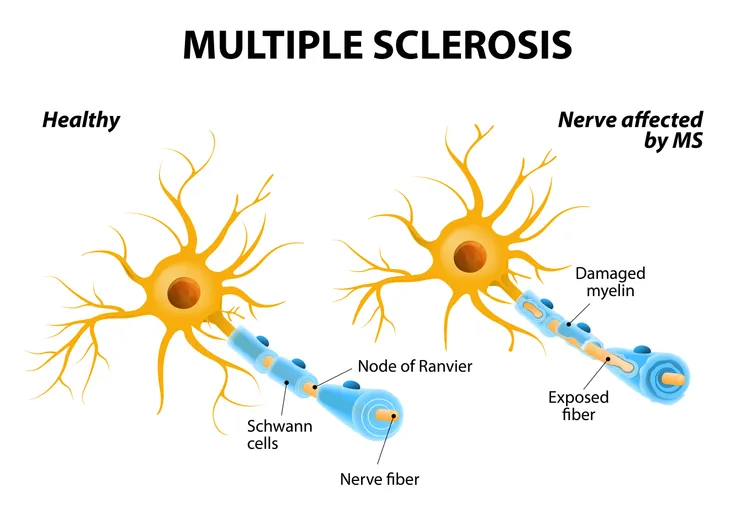
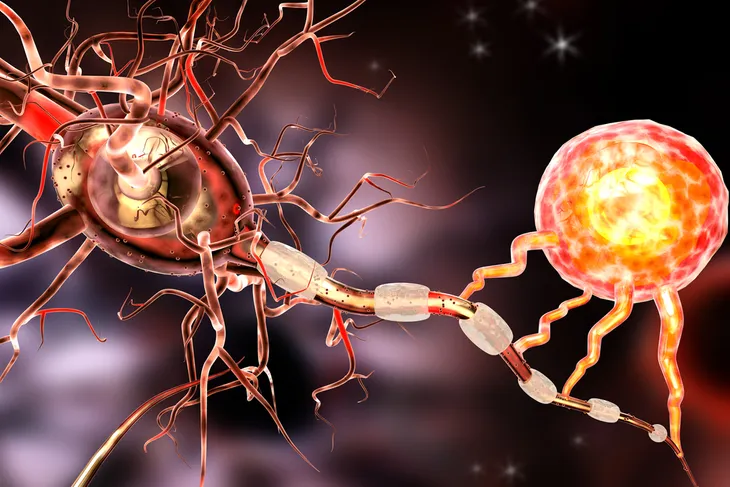
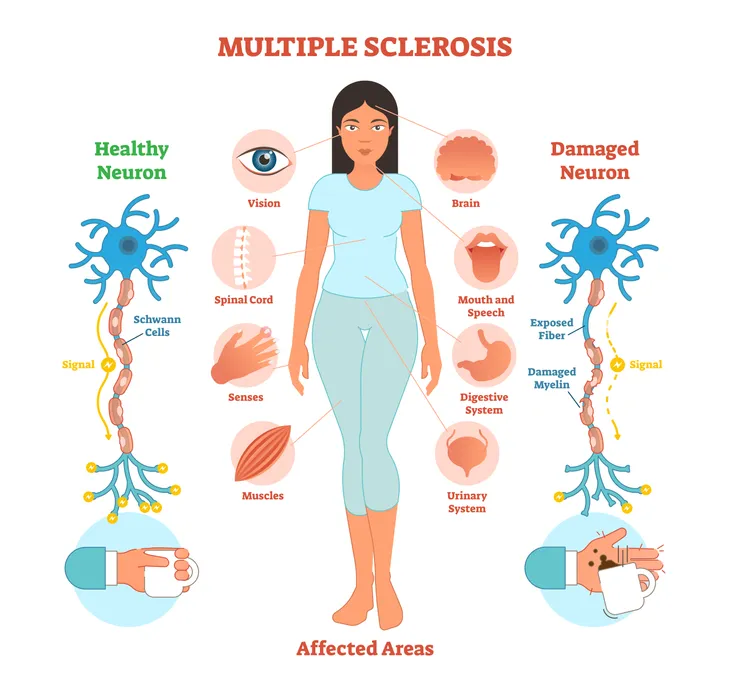
Similar to NMO, MS is also an autoimmune disease that affects the central nervous system, including the brain and spinal cord. “The disease attacks myelin, the protective covering of the nerves, causing inflammation and often damaging the myelin,” writes the MS Society of Canada. The attack on the protective layer of our nerves causes inflammation and often damages the myelin which is necessary “for the transmission of nerve impulses through nerve fibers.” If the damage isn’t too severe, these nerve impulses will still be able to travel through the fibers without too much interruption. However, if the damage is severe and scar tissue ends up replacing the myelin, the nerve impulses will be “completely disrupted, and the nerve fibers themselves can be damaged,” explains the source.
This disease is totally unpredictable and can result in a slew of symptoms including extreme fatigue, lack of coordination, weakness, tingling, impaired sensation, vision problems, bladder problems, cognitive impairment, and even mood changes, says the MS Society of Canada. Patients and family members feel the effects of this disease as they are far and wide, causing physical, emotional, and even financial distress.
Now that we understand what both of these conditions are on their own, let’s start talking about what they might have in common, as well as their differences.
They are Both Nerve Conditions
One reason people often mix up MS and NMO is because they are both nerve conditions. Both conditions attack the central nervous system. According to the Mayo Clinic, they are so similar that, for about 100 years, NMO couldn’t be distinguished from MS. In fact, due to the similarities in the two, Healthline says scientists once believed NMO might be a form of MS.
“In NMO and MS, the immune system reacts against the body in what are often termed episodes or attacks,” explains the Mayo Clinic. “These episodes cause inflammation and destruction of cells.” As we previously explained, NMO targets the optic nerves and the spinal cord, which are also commonly affected in MS. This is another major similarity between the two.
NMO Symptoms
One of the biggest differences between NMO and MS are the symptoms, particularly the speed at which they appear. NMO is a rare disease that causes damage to the optic nerve, brain stem, and spinal cord. “It leads to optic neuritis, which causes pain in the eyes and loss of vision. Other symptoms can include muscle weakness, numbness, and bladder control problems,” explains Healthline.
In addition to their differing symptoms, the Mayo Clinic explains that the rate in which these symptoms occur is also unique. NMO patients “often have severe, rapidly worsening symptoms.” Healthline also points out that the attacks of NMO can lead to serious health complications that cannot be reversed. For example, when the optic nerves are affected, it can cause blindness. Similarly, when the spinal cord is affected, it can lead to paralysis, loss of bladder control, and even breathing difficulties that can become fatal, says the Mayo Clinic. Patients with NMO may also have episodes of vomiting that last up to a month, which is not one of the symptoms of MS.
Early and aggressive treatment is the best way to combat the symptoms of NMO, says Healthline.
MS Symptoms
On the other hand, the beginning stages of MS are typically quite mild and not life threatening. The symptoms of MS are not quite as severe as NMO, particularly in the early stages. However, the effect of these symptoms over time can become quite serious. “Over time, patients with multiple sclerosis may develop disabilities including paralysis (most typically in the legs), but permanent disability often tends to develop gradually and not as a result of sudden attacks as it does in NMO,” says the Mayo Clinic.
Similar to NMO, MS attacks the entire central nervous system and can affect the optic nerve, spinal cord, and brain. “The symptoms include numbness, paralysis, vision loss, and other problems,” writes Healthline. “Severity varies greatly from person to person.”
The Nature of Both Diseases
While the symptoms of these two conditions differ, as well as the speed, they do follow a similar course, says Healthline. Some people who have MS will experience remitting episodes, in other words, their symptoms come and go. Patients with NMO will also experience something similar to this. Their symptoms come in the form of “attacks” that return on a regular basis.
However, there are differences. The source adds that NMO may only strike once and last for a month or two, whereas “some types of MS don’t have periods in which symptoms go into remission. In these cases, symptoms simply get progressively worse over time,” writes Healthline. NMO doesn’t follow a progressive course like MS. The symptoms of NMO only occur in “attacks.”
Brain Scans
Yet another different between patients with NMO and MS is what shows up in their brain scans. Patients with NMO will have normal results from a magnetic resonance imaging (MRI) brain scan, particularly in the early stages of their disease.
On the other hand, patients with MS patients will have some abnormalities. In addition to this, according to the Mayo Clinic, 80-percent of patients with NMO will have “distinct, long lesions on the spinal cord on MRI that aren’t present in patients with multiple sclerosis.”
Unique Antibodies
According to researchers at the Mayo Clinic, patients with NMO have “both a unique antibody associated with NMO and the target cell that the antibody destroys.” Antibodies that have been activated by the immune system are used to fight off infections. “The antibody, called NMO-immunoglobulin G (NMO-IgG), is present in 70-percent of patients with NMO,” writes the source.
So, what does this have to do with MS? Well, this is yet another area where these two conditions differ. Patients with MS do not have NMO-IgG.
Diagnosis
There are ways to diagnose both MS and NMO, but as a result of the NMO-IgG antibody, it’s easier to get an early and accurate diagnosis of NMO than it is for MS. After discovering this antibody, researchers developed a blood test that can help provide an efficient and accurate diagnosis of NMO. This was a major accomplishment for NMO, because early treatment is the key to an improved outcome.
Unfortunately, for patients with MS, there is no blood test to help with an early diagnosis. In fact, according to the Mayo Clinic, there are no specific tests that can be used for a definitive diagnosis of MS. However, there are a variety of other tests (e.g., blood test, MRI scan, lumbar puncture, or evoked potential tests) that can help doctors rule out other conditions that might produce similar signs and symptoms. This is called a differential diagnosis.
Prevalence of MS
We touched on this briefly earlier on, but another major distinction between MS and NMO is the prevalence of each. MS is much more common than NMO. The National MS Society reports that nearly 1-million people in the United States are living with MS. These results were found in a recent study and ended up being twice as high as what researchers originally estimated based on a previous study.
Healthline adds that people with MS tend to live farther away from the equator. For example, Canada has one of the highest rates of MS in the world, with an estimated 1 in every 385 Canadians living with this disease, says the MS Society of Canada. “While it is most often diagnosed in young adults aged 20 to 49, younger children and older adults are also diagnosed with the disease.”
Prevalence of NMO
Unlike MS, cases of NMO can be found in any climate. “NMO occurs in all parts of the world and may be the most common form of demyelinating disease in certain populations such as Africans, Asians and Native Americans,” writes the National Multiple Sclerosis Society. Another difference is that unlike MS, NMO is considered a rare disease. It is estimated that there are about 250,000 cases around the world, adds the source, including 4,000 in the United States.
It’s important to note that both MS and NMO are known to be more common in women than men, says Healthline. The exact estimate provided by National Multiple Sclerosis Society for NMO is that it’s 80-percent more prevalent in women compared to men. NMO can be diagnosed at any age (in children as young as 3 and adults as old as 90), but it’s most often found in adults aged 40 to 50.
Reaction to Medications
Both NMO and MS are incurable, but that’s about their only similarity when it comes to treatment. The Mayo Clinic explains that MS is initially treated with interferon beta medications that work to reduce inflammation. These medications won’t help patients with NMO. In fact, they could actually end up doing more damage and cause more severe attacks.
According to Healthline, because NMO often returns after the first episode, patients are prescribed immunosuppressive medications such as azathioprine, mycophenolate mofetil or rituximab. These medications will help prevent future attacks. “Randomized clinical trials are beginning to assess the efficacy and safety of a variety of immunotherapies in treating NMO,” adds the source.
For those who don’t respond well to initial therapies, they may undergo plasma exchange, “where antibodies are removed from the bloodstream,” writes the Mayo Clinic. “When plasma exchange is administered soon after an attack, patients may regain vision if blindness has occurred (or movement in the case of paralysis).” Early treatment is necessary because if the treatment is delayed by even just a few months, those functions can’t be restored.
When it comes to MS, patients are prescribed medications that help reduce any flare-ups associated with their symptoms, as well as underlying causes of the disease.