With no understanding of why it happens or how to cure it, type 1 diabetes (T1D) remains one of the largest autoimmune mysteries to date affecting over 1.25 million Americans every year. As a result, there are a lot of myths and misconceptions surrounding the diabetes community, and many of them just aren’t true! Not surprisingly, it can be difficult to know what to believe and what not to believe when it comes to type 1 diabetes.
Parents with T1D Automatically Pass it on to Their Children
If parents have 1 diabetes, there is a higher chance that their child will have type 1 diabetes, says WebMD. There’s no getting around this. This is especially true if the father has type 1 diabetes, and even more so if both parents have it. However, there is no guarantee that type 1 diabetes will be passed down from parent to child.
Type 1 and Type 2 Diabetes are the Same
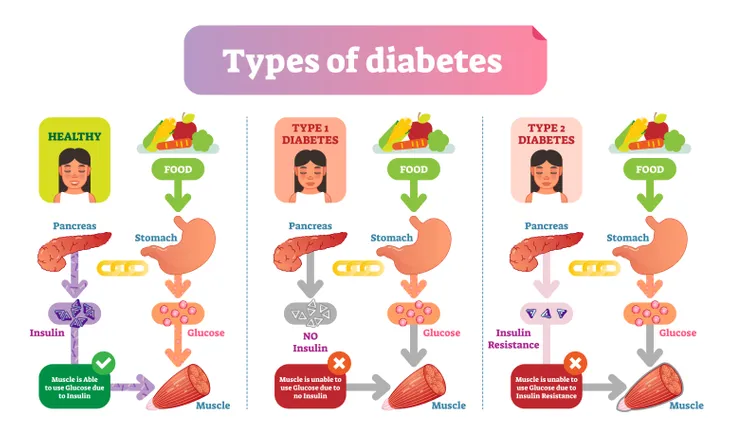
Many people aren’t able to differentiate between type 1 diabetes and type 2, but the reality is they are very different. People with type 1 diabetes aren’t able to produce their own source of the hormone that allows them to use glucose for energy due to their body attacking certain cells within the pancreas. People with type 2 diabetes can produce this hormone but don’t respond to it. Their bodies also tend to not be able to produce enough of the hormone down the road. Type 2 diabetes can also be caused by lifestyle and dietary choices, whereas type 1 diabetes can not.
People With Type 1 Diabetes Can’t Eat Sugar
It is true that people with type diabetes have to think more about what they put in their mouths, but that doesn’t mean that they can’t eat sugary foods entirely, explains Diabetes Australia. As long as after eating people with type 1 diabetes take enough of the hormone that allows them to use glucose for energy to keep their blood sugar levels in a healthy range, they can pretty much eat whatever they want. (Learn more with these Diet Tips for Type 1 Diabetes).
There are even apps that people with type 1 diabetes can use to keep track of the foods they eat; specifically, the carbohydrates as they are what usually cause the spikes in blood sugar.
Treatment Gives You The Freedom to Eat Whatever You Want
As described above, type 1 diabetes treatment is effective to the point of allowing for the consumption of just about any kind of food. However, some foods are better than others for managing blood sugar levels. These foods include nutritious, low-fat, high-fiber foods such as fruits, vegetables, and whole grains (as well as any other foods recommended by a doctor or dietician).
Plus, due to the fact that type 1 diabetics are more susceptible to cardiovascular problems like coronary artery disease, heart attack, stroke, and high blood pressure, adhering to a healthy diet is especially important.
People with Type 1 Diabetes Aren’t Able to Live a Normal Life
By understanding how foods affect blood sugar levels and adhering to treatment rules, people with type 1 diabetes can live as full of a life as anyone else. For example, it’s completely normal for children with type 1 diabetes to play sports and participate in extracurricular activities, just like any other children. The only modification that might need to be made is having a sugary snack on hand in case their blood sugar drops on account of physical activity.
There is Only One Form of Treatment for Type 1 Diabetes
While hormone treatment is currently the only form of treatment for the majority of people dealing with type 1 diabetes, there have been many advancements in the past 10 years in how this treatment is administered. One such advancement is the pump – a smartphone-sized device that attaches to the outside of the body with a tube that inserts under the skin of the stomach. This tube then automatically administers specific amounts of the rapid-acting form of the hormone based on meals eaten and corresponding blood sugar levels.
Another modern development is continuous glucose monitoring (CGM) wherein, similar to the pump, a monitor is attached to the body using a fine needle just under the skin that checks blood glucose level every few minutes. However, CGM is not yet considered to be as accurate as standard blood sugar monitoring, so checking your blood sugar levels manually is still recommended.
It is worth noting, however, that for many people, these modern advancements in type 1 diabetes treatment are still too expensive to adapt.
Type 1 Diabetes is Caused From Too Much Sugar
While it’s not entirely understood what causes someone to get type 1 diabetes, it is known that it’s not caused by lifestyle factors like eating too much sugar, says WebMD. In fact, when blood sugar levels dip too low in people with type 1 diabetes, eating sugar is actually required to bring levels back into a normal range.
Type 1 Diabetes is Caused From Poor Lifestyle Choices
Again, type 1 diabetes is not caused by poor lifestyle or dietary decisions. Poor lifestyle or dietary decisions are only a risk factor for type 2 diabetes, explains Diabetes Australia. However, unhealthy living certainly doesn’t alleviate the symptoms associated with type 1 diabetes and can lead to a poorer quality of life. Higher susceptibility to certain health problems like heart attack and stroke should also encourage people with type 1 diabetes to live a healthier lifestyle.
Treatment for Type 1 Diabetes is Predictable
Here’s a glimpse into the many things that can influence blood sugar levels:
- Food
- Stress
- Hormone changes
- Periods of growth
- Illness
- Physical activity
Even when following a strict meal and dosing schedule, any one or combination of things above can result in blood sugar levels fluctuating unpredictably. While this is completely natural, it also explains why constant monitoring is so important, regardless of how familiar someone is with what they’re eating or what they’re doing.