- 4.5 million Americans will need a blood transfusion each year.
- This life-saving procedure replaces lost blood from surgery or injury. Individuals with conditions like anemia or cancer may also require blood transfusions.
- Blood transfusions are usually very safe and strict procedures are in place to ensure testing, handling, and storage of donated blood is as safe as possible. However, some risks are still possible.
A blood transfusion is a life-saving procedure that can help replace lost blood from injury or surgery. Blood transfusions may also be necessary for individuals suffering from illnesses that prevent their bodies from making blood. But there’s a lot more to know about it. Understanding what it is, the different types, who they’re for, as well as the benefits and risks, is the best way to get informed.
What Are Blood Transfusions?
A blood transfusion is a common medical procedure that involves administering donated blood to a patient through an intravenous line (IV). Blood transfusions are commonly used to “replace blood and blood components that may be too low,” says the Cleveland Clinic.
Blood transfusions can also be life-saving as they can replace lost blood caused by surgery or a serious injury. They’re also used for a variety of other reasons that we’ll explain in more detail later.
Autologous Blood vs. Donor Blood: What’s the Difference?
If you need a blood transfusion, it’s important to know that blood can be provided from two sources. They are autologous blood that uses your own blood, or donor blood which as you guessed it, is donated blood from another individual.
If you have surgery coming up, your doctor may recommend a pre-operative donation, which means a blood bank will draw your blood and store it until it’s needed during or after surgery. In some cases, like emergencies, doctors will need to rely on blood donations from volunteers.
Types of Blood Transfusions
The American Red Cross explains there are four common types of blood transfusion,s including red blood cell transfusions, platelet transfusions, plasma transfusions, and whole blood transfusions. Here’s what they mean:
- Red blood cell transfusions are typically used for individuals suffering from an iron deficiency or anemia which means they don’t have enough red blood cells.
- Platelet transfusions are used for patients who have low platelet counts.
- Plasma transfusions are used for patients with serious burns, severe infection, or liver failure.
- Whole blood transfusions are used for patients who require red blood cells, white blood cells, and platelets.
Who Needs Blood Transfusions?
Blood transfusions are more common than you may think. The Community Blood Center says 4.5 million Americans will need a blood transfusion each year. But who needs them exactly?
Blood transfusions are necessary for anyone who “lacks enough blood to function properly,” explains Medical News Today. They’re commonly used if an individual loses blood during surgery or if an individual has sustained a severe injury such as a car crash, notes the source. Certain conditions may also require blood transfusions ,such as anemia, hemophilia, cancer, sickle cell disease, kidney disease, and liver disease.
The Benefits of Blood Transfusions
Blood plays a vital role in the body. For starters, it transports oxygen and nutrients to all parts of the body. Blood also carries waste materials to the lungs, kidneys, and digestive system to be removed from the body, and it helps fight infections. Finally, blood also plays a role in carrying hormones around the body.
The biggest benefit of a blood transfusion is providing your body with sufficient blood or one of the components of blood. Without it, you could face a life-threatening situation, says the Cleveland Clinic.
What to Expect Before a Blood Transfusion
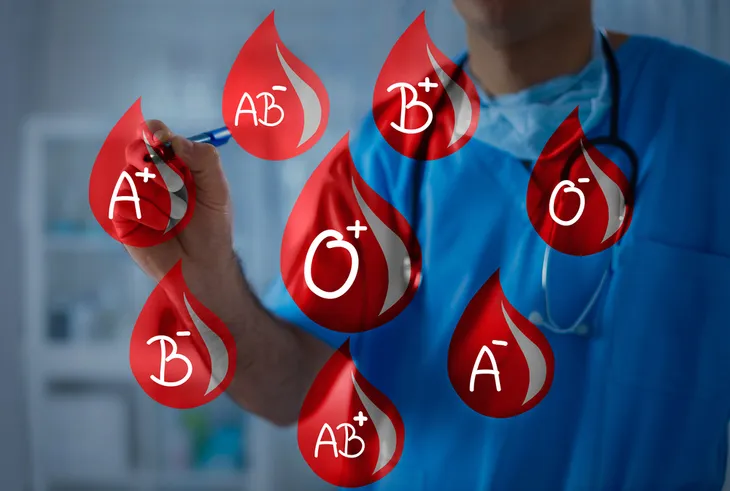
Before receiving a blood transfusion, a technician will first need to test your blood to determine your blood type (A, B, AB, or O and Rh-positive or Rh-negative). To do this, they will prick your finger with a needle to get a couple of drops of blood, or they may draw blood from one of your veins.
It’s important to know your blood type before the transfusion because receiving the wrong type can cause antibodies in your blood to attack the new blood. As a result, you can become sick.
Furthermore, dietary and lifestyle changes aren’t usually necessary before a blood transfusion; however, follow the advice of your doctor.
What to Expect During a Blood Transfusion
Blood transfusions usually take place in a hospital or clinic. However, if necessary, Medical News Today says nurses may be able to perform transfusions at home.
To receive a blood transfusion, a medical professional will place a small needle into your vein (usually in the arm or hand). Then blood will transfer from a bag through a rubber tube and into your veins. Transfusions typically take 1 to 4-hours however the time will vary depending on several factors like how much blood you need. During the transfusion, your vital signs will be carefully monitored.
What to Expect After a Blood Transfusion
The recovery time may vary depending on the reason for your blood transfusion. That said, Medical News Today notes individuals can be discharged in less than 24-hours after the transfusion.
After the procedure, you may feel tenderness in the arm or hand. In some cases, bruising may develop at the site of the needle. If you develop any unusual symptoms such as nausea or difficulty breathing after the procedure be sure to inform the doctor right away. Reactions are possible although rare.
Possible Risks
First, we want to point out that blood transfusions are usually very safe. Medical News Today emphasizes that “strict procedures exist to ensure that the testing, handling, and storage of donated blood is as safe as possible.” That said, as with all procedures, there is a chance your body can react to new blood.
Some reactions occur immediately, while others can have a delayed reaction that develops several days after the procedure. One possible risk is a fever. Fevers are not usually serious unless they’re accompanied by chest pain or nausea. If this occurs, notify your doctor right away.
Next, we’ll take a look at a few other possible risks you should be aware of.
Allergic Reactions
The most common adverse reactions from a blood transfusion are allergic and febrile reactions, says the Centers for Disease Control and Prevention (CDC). In fact, these reactions make up over half of the reported reactions to blood transfusions, says the source.
Allergic reactions can vary from mild to severe. Some common symptoms to look out for include chest or back pain, trouble breathing, nausea, fever, chills, low blood pressure, and a rapid pulse. If a reaction occurs, the nurse or doctor will stop the transfusions right away, determine how severe the reaction is, and what treatments are needed.
Hemolytic Reactions
Another possible risk of blood transfusions is a hemolytic reaction. This may occur if the blood types are not compatible, which causes “the immune system to attack the new blood cells,” explains Medical News Today.
A hemolytic reaction is serious, however, it is very rare. Common symptoms of a hemolytic reaction include lower back pain, chest pain, fever, nausea, and dark urine, says the source. Notify your doctor immediately if you develop any of these symptoms.
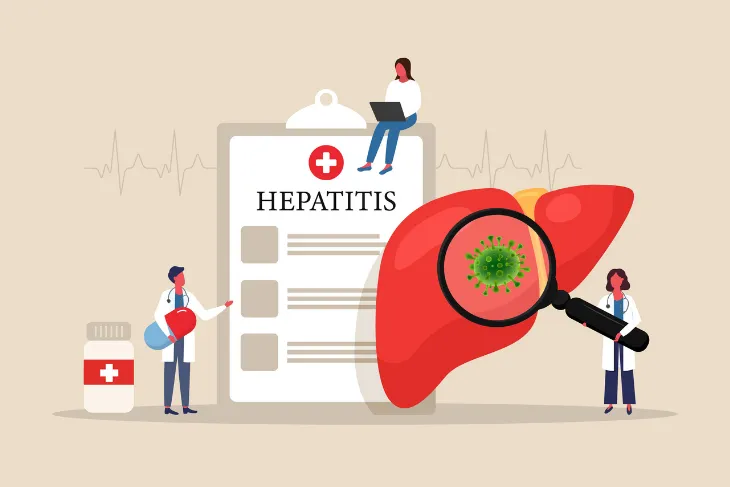
Are Infections Possible?
Although extremely rare, donated blood may cause an infection caused by bacteria, viruses, or parasites in the blood. Possible infections include hepatitis B, C, or HIV. But it’s important to note that “all blood for transfusion is tested for evidence of certain infectious disease pathogens,” explains the CDC.
Due to these critical tests, the chance of an individual contracting hepatitis B from a blood transfusion is 1 in 300,000, and the chance of contracting hepatitis C is 1 in 1.5 million. The American Red Cross also says, “There is a 1 in 2 million chance that donated blood will not only carry HIV but also infect a transfusion recipient.”
How to Become a Blood Donor
As you can see, blood transfusions are life-saving procedures. The Community Blood Center says someone needs blood every 2-seconds. About 37-percent of the American population is eligible to donate blood but only 10-percent do so annually. The good news is, becoming a blood donor is easy.
To be eligible to donate blood in the U.S. you must be at least 16-years old, weigh at least 110-pounds, and be in good health. There are a few other requirements too, which you can find on the American Red Cross’s website. If you’re eligible, search for a local donation clinic near you. You could save a life!