Those with digestion issues such as Irritable Bowel Syndrome (IBS) know all too well the discomfort of abdominal pain, intestinal gas and bloating that can occur after eating certain foods.
The low-FODMAP diet — sometimes referred to simply as the FODMAP diet — is an eating plan specifically designed to help people manage the symptoms of IBS. Developed by a group of Australian research scientists, it has been proven extremely effective in reducing IBS symptoms when followed correctly.
Common IBS Symptoms
IBS is currently thought to affect between 25 and 45 million Americans and 10 to 15 percent of people worldwide. The broad range of possible IBS sufferers reflects the fact that many people who have the disease have not been diagnosed.
The symptoms of IBS include:
- Stomach pain or cramping
- Constipation
- Diarrhea
- Bloating
- Irregular bowel movements
- Disturbed sleep
- Anxiety
- Depression
The symptoms of IBS vary dramatically from one patient to the next and are often inconsistent. As such, many may chalk their symptoms up to an upset stomach or some other transient issue. This is why many people who have IBS are undiagnosed.
IBS Causes
The precise cause of IBS is not fully understood. However, there is a strong indication that people who suffer from the condition have developed it as a result of hypersensitivity to certain foods, which cause an adverse reaction in the gut. This is where the low-FODMAP diet comes in.
Before giving the low FODMAP diet a try, here are six important things to know.
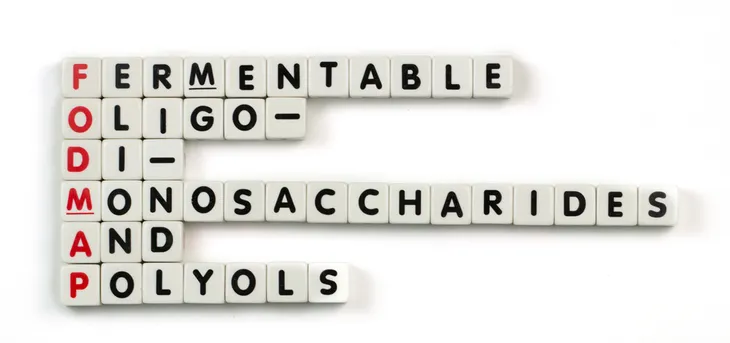
What Are FODMAPs?
FODMAP is an acronym used to describe certain carbohydrates—specifically the short-chain variety—found in foods. According to FodmapFriendly.com, it stands for:
- Fermentable
- Oligosaccharides
- Di-Monosaccharides
- and
- Polyols
In those who suffer from digestion problems like IBS, the International Foundation for Functional Gastrointestinal Disorders says FODMAPs “are poorly absorbed in the small intestine and rapidly fermented by bacteria in the gut.” When this occurs, food may remain in the gut for too long and begin to ferment. This fermentation can cause bloating, discomfort, and the other gastrointestinal issues associated with IBS.
Common FODMAPs
Avoiding FODMAPs can be helpful for people suffering with IBS. However, cutting them out of your diet completely can be tricky because they are found in an extremely wide variety day-to-day foods. Fructose is one FODMAP carbohydrate to stay away from, and is commonly found in things like fruits, vegetables and honey.
It’s recommended that those on a low FODMAP diet also refrain from eating legumes like beans, lentils and soy, which contain carbohydrates called galactans. Polyols—from stone fruits like avocado, cherries and peaches, as well as any sweeteners containing sorbitol, mannitol, xylitol or maltitol—should be avoided as well.
Dietary Culprits
Here are some other main dietary culprits:
- Oligosaccharides: Legumes, rye, wheat, blueberries, pear, watermelon, nectarines, garlic, leek, onions, and scallions.
- Disaccharides: Lactose-rich foods like milk, yogurt, cheese, and other dairy products.
- Monosaccharides: Canned fruits, jams, honey, certain breakfast cereals, and fruits such as figs, mangoes, apples, dates, sultanas, grapes, kiwi, and bananas.
- Polyols: Low-calorie sweeteners used as additives in gum, sweets, and low-carb foods, lychee, blackberries, and various other fruits and vegetables.
Who Is The Diet For?
A low FODMAP diet is primarily used to help those with IBS, but it can also be beneficial for people with functional gastrointestinal disorder and certain autoimmune diseases like rheumatoid arthritis, multiple sclerosis, eczema and fibromyalgia. For people who suffer with IBS and other gastric sensitivity disorders, the benefits of following a low-FODMAP diet are well documented. In fact, research has shown that cutting out FODMAPs can greatly reduce or eliminate IBS symptoms in 86 percent of people.
The digestive symptoms associated with IBS can be debilitating. Alarmingly, one large-scale study found that people who suffer with IBS would, on average, trade 25 percent of their remaining lives in exchange for living without symptoms.
While most people are able to easily digest FODMAPs, individuals with these conditions can be particularly sensitive to them. Stomach pain and bloating are two of the worst and most common symptoms associated with IBS and other inflammatory bowel diseases. Evidence suggests that adopting a low-FODMAP eating plan can dramatically reduce these symptoms. Where stomach pain is concerned, following a FODMAP diet gives you an 81 percent chance of improved symptoms. As for bloating, a FODMAP diet gives IBS sufferers a 75 percent chance of improvement.
Overall, studies consistently demonstrate that a low-FODMAP diet can significantly improve quality of life in several ways, though more research in this area is required.
How It Works
Low-FODMAP diets are not intended as a long-term eating plan. The diet should be adopted in phases, starting with strict avoidance of certain foods before moving towards gradual reintroduction.
The phases of a FODMAP diet work as follows:
Stage 1: Total Restriction
During this stage, all high-FODMAP foods must be eliminated from the diet.
This restriction should last between three and eight weeks. The precise timeframe will be determined by how quickly an improvement in symptoms occurs. For some people, this may take up to eight weeks, while others experience a noticeable difference in a week or less.
Stage 2: Reintroduction
Stage two involves the gradual reintroduction of FODMAPs. It is important to include at least some FODMAPs in the diet to maintain a proper balance of gut bacteria.
The aim of this stage is to determine:
- Which FODMAPs cause symptoms
- Which FODMAPs do not cause symptoms
- How much of specific FODMAPs can you tolerate
During stage two, dieters must reintroduce each high-FODMAP food individually and for a period of three days. Keeping a careful eye on symptoms during this testing phase will illustrate which foods trigger your IBS and to what degree.
Many people go wrong during this phase by continuing to eat a certain food if their three-day test does not produce symptoms. Even if you experience no adverse effects when reintroducing a specific FODMAP source, you must cut it out entirely when moving onto the next test. Otherwise, you cannot be sure which food you are reacting to when adverse symptoms occur.
Stage 3: Personalizing Your Diet
In this final stage, you will adopt your new, customized low-FODMAP diet. According to the outcome of stage two, you can reintroduce any high-FODMAP foods identified as “safe” while restricting all those that caused IBS symptoms. It is important to closely regulate the amount of each reintroduced food you consume, as going overboard with any one item could lead to an IBS flare-up, even when one was not observed during the testing phase.
Keep in mind that food intolerances can change over time. This means there is a chance you may become sensitive to a food that was previously identified as “non-triggering” in stage two. If this happens, return to stage one of the diet and repeat the process from the top.
Common Pitfalls
As with many diets, there are common low FODMAP diet pitfalls that can hinder its effectiveness. One such pitfall, according to the International Foundation for Functional Gastrointestinal Disorders, is over-limiting your diet. To avoid lactose, for instance, many people will remove all dairy products from their diet, but this is unnecessary. “You can continue to use low-lactose milk products such as aged cheeses and lactose-free yogurt on a low FODMAP diet,” the source says, unless the person is vegan or has an allergy to milk.
Another common pitfall is not getting enough fiber while on the low FODMAP diet. This tends to happen as a result of eliminating so many foods from the diet, but fiber is important for gut health. Seek out low FODMAP fibers—which can be found in certain fruits, vegetables and grains—as the source says they are “fermented more slowly and are less likely to disrupt fluid balance in the gut.”
Low FODMAP Diet for IBS
Although a low FODMAP diet has helped those with conditions like functional gastrointestinal disorder, multiple sclerosis and fibromyalgia, most of the research to-date has been on patients of IBS.
In a 2014 study, for instance, 30 people with IBS were put on a low FODMAP diet for 21 days. During this time, participants saw a 50-percent decrease in symptoms such as bloating, abdominal pain and gas. A low FODMAP diet may not be appropriate for everyone with IBS, however, so it’s important to speak to a physician and find a registered dietitian who can help you manage the elimination diet prior to trying it.
When to Speak to a Doctor
Speak to your doctor if you think you may be suffering with IBS. There are other, far more serious conditions which can cause IBS-like symptoms, including celiac disease and colorectal cancer. Once other possible causes have been ruled out, your doctor will be able to advise you whether adopting a low-FODMAP diet is an appropriate course of action.