- Following the renal diet helps people with chronic kidney disease slow the progression to end-stage renal failure and improve kidney functioning.
- The renal diet must be developed and monitored by your doctor or a dietician.
- Standard guidelines include limiting sodium, potassium, protein, and phosphorus.
- Limiting fluid intake is also sometimes necessary.
The renal diet is for people with compromised kidney function, usually due to chronic kidney disease. The condition most often affects people with high blood pressure or diabetes.
Around 37 million American adults have chronic kidney disease. Unfortunately, approximately 40% of people with severe kidney problems aren’t aware they have them. Symptoms may include itching, decreased urination, or swelling of the feet and ankles. Muscle aches, unexplained fatigue, and sleep problems are also potential signs of chronic kidney disease.
If you’re diagnosed with chronic kidney disease, your doctor will likely prescribe medications, monitoring, and a renal diet as courses of treatment.
What Is the Purpose of the Renal Diet?
The renal diet aims to reduce waste levels in the bloodstream. When kidney function has been compromised, waste isn’t filtered as effectively. Any waste that’s allowed to build up in the bloodstream can negatively affect electrolyte levels.
Electrolytes are minerals that are essential for your body to function properly and significant health issues can arise from an electrolyte imbalance. For example, electrolyte imbalances can result in heart problems, bone deterioration, and new-onset seizures.
Each Renal Diet Is Unique
Although all renal diets follow similar basic guidelines, each person requires a customized plan. For this reason, it’s essential to consult with your doctor or a specialized dietician to have a renal diet created for you.
The exact amounts of restricted nutrients (like sodium or potassium) will vary based on a range of factors. Your doctor will take your age, weight, stage of renal failure, and other health conditions into consideration.
Your Renal Diet May Change
As kidney disease progresses, your dietician or doctor will likely change your renal diet’s limitations and restrictions. Changes may also be necessary as you age or if you experience significant weight fluctuations.
In some cases, changes may be made when the renal diet doesn’t appear to be working the way it’s supposed to. If kidney health isn’t improved, further restrictions could be necessary.
 novak.elcic / Shutterstock
novak.elcic / ShutterstockChoose Less Sodium
High blood pressure is a common concern in those with CKD. Studies found decreasing sodium intake helps lower systolic and diastolic blood pressure in people with kidney disease. Lower sodium intake also decreases proteinuria, which increases levels of protein in the urine. Proteinuria happens when protein spills from the kidneys and is common in chronic kidney disease.
Ways to Restrict Sodium Intake
Sodium is a mineral that, along with chloride, creates table salt. It’s added to many prepackaged foods, so buying fresh when possible can help naturally reduce sodium intake.
When cooking your meals, try to use other herbs and spices to add flavor to meals instead of salt. Experiment with seasonings like garlic, black pepper, lemon zest, chili powder, and onion powder. Store-bought seasoning mixes should be used sparingly, as they often contain salt.
Salt is also used to help preserve canned foods such as meats, vegetables, and beans. Rinse all canned foods with water before eating or cooking them to help remove excess sodium.
Read food labels on everything you purchase and look for phrases that indicate that it’s safe for a sodium-restricted diet. Examples of these phrases include:
- Sodium free (or salt-free)
- Low sodium (or low salt)
- Reduced sodium (or reduced salt)
- Unsalted
- Lightly salted
Reduce Protein Intake
One of the kidney’s most important functions is eliminating the waste products caused by protein metabolism. By reducing how much protein you consume, the kidneys process less waste. Processing less waste helps protect already-damaged kidneys.
Protein is still an essential nutrient for the body, so you shouldn’t avoid it entirely. Instead, try to eat small portions of high-quality protein. Learning the correct portion sizes for different protein types can be helpful.
Proper portion sizes include:
- Cooked meat, chicken, or fish: 2 to 3-ounces
- Milk or yogurt: 1/2-cup
- Cooked beans: 1/2-cup
- Cheese: 1 slice
- Nuts: 1/4-cup
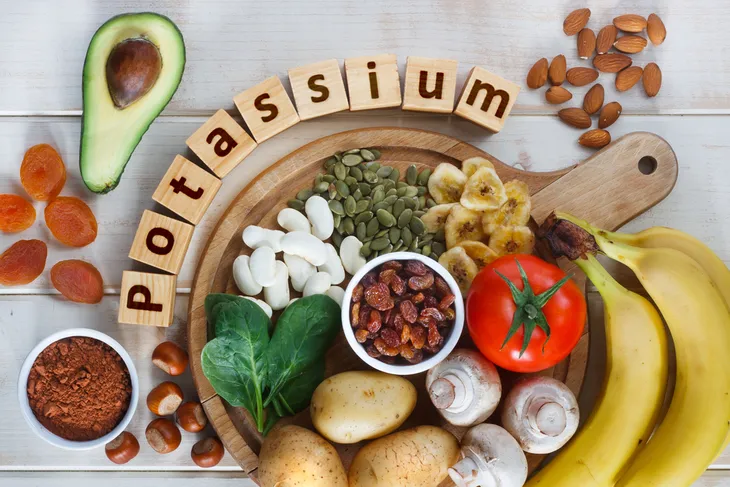
Be Careful With Potassium
Hyperkalemia, a condition where there’s too much potassium in the bloodstream, is common in people with chronic kidney disease. The condition can affect people with any stage of renal failure, including those with very mild kidney problems.
Damaged kidneys don’t excrete potassium correctly, which allows it to build up in the bloodstream. In turn, high potassium levels can damage the body’s nerves and muscle cells, including those in your heart. Limit your potassium intake to help reduce the risk of hyperkalemia.
Certain foods contain higher-than-average amounts of potassium and should be avoided. Beware of salt substitutes, which are often very high in potassium. Always read labels to verify a product falls within safe renal diet guidelines.
You should also avoid or strictly limit:
- Oranges (including orange juice)
- Bananas
- Potatoes
- Tomatoes
- Brown or wild rice
- Bran cereals
- Dairy foods
- Whole wheat bread and pasta
- Beans
- Nuts
Choose These Low Potassium Foods Instead
Your body still needs some potassium to function. Choose foods that contain potassium in lower amounts. Start by switching your morning orange juice for apple, grape, or cranberry juice.
Other low-potassium foods include:
- Apples
- Peaches
- White bread or pasta
- White rice
- Unenriched rice milk
- Cooked rice cereals (like farina)
- Cooked wheat cereals (like grits)
Be Cautious With Phosphorus Levels
Your doctor will regularly check calcium and phosphorus blood levels if your kidneys are damaged. Even in the earliest stages of kidney disease, phosphorus levels can get too high.
The problem with high phosphorus levels is they cause calcium levels to drop. When this happens, the body pulls the calcium it needs from your bones, making them weak and brittle. While many foods contain phosphorus, dairy foods contain exceptionally high amounts.
You May Need to Watch Your Fluids
In the early stages of kidney disease, it isn’t necessary to monitor your fluid intake. However, if kidney failure has progressed or you’re receiving dialysis, you’ll need to watch your fluid consumption.
Fluid consumption doesn’t only pertain to water and other liquids. Fluid-rich foods like popsicles, watermelon, or soup also count toward your daily totals.
Fluids need to be monitored, as they’ll build up in the body and cause issues such as shortness of breath. In some cases, this can lead to life-threatening emergencies. Your doctor or dietician will tell you exactly how many fluids (usually in ounces) you can have daily.
Consider Antioxidants
A study by the National Institute of Health suggests antioxidants may help prevent progression to end-stage renal failure. You should talk to your doctor first, but generally, adding antioxidant-rich foods to your diet could be a good idea.
Cranberries, red grapes, and apples are excellent antioxidants that are generally safe for those on renal diets. Additional sources of antioxidants usually considered safe include peaches, raspberries, and blueberries.
Slow the Progression of Chronic Kidney Disease
When followed correctly, the renal diet can help slow the progression of chronic kidney disease. It could also help promote better kidney functioning, which generally improves your quality of life.
It’s important to continue following your renal diet, even if you begin feeling better. Deviating from the diet could cause further damage to the kidneys or faster progression to end-stage renal failure.