Your digestive system holds the key to your health. If you don’t believe me, look at the medical research that considers your gastrointestinal tract far more than your body’s plumbing system.
In fact, Michael Gershon, professor of anatomy and cell biology at Columbia University, New York, considers the gut the root of health, which means if the delicate balance of flora in the gut is thrown off—it can result in a domino effect of ill health—including chronic bloating, irritable bowel syndrome, depression, osteoporosis, and chronic migraines.
So let’s explore the finely tuned, intricate system, known simply as the gut…
Humans Are Walking Bacterial Colonies
I’ll bet you never considered yourself “a walking bacterial colony.” However, scientists point out that our guts contain more microbial genes than human genes. We don’t start out that way, of course.
As unborn fetuses, the intestines are sterile and we’re protected by our mothers, however, once born, our intestines begin to collect and house trillions of microbiota to aid food digestion, vitamin absorption, and power our immune systems.
However, a large body of scientific research also points out that an over-prevalence of certain microbiota can also lead to certain chronic health conditions, including autism, colitis, obesity, and several mood conditions.
What Enterotype Are You?
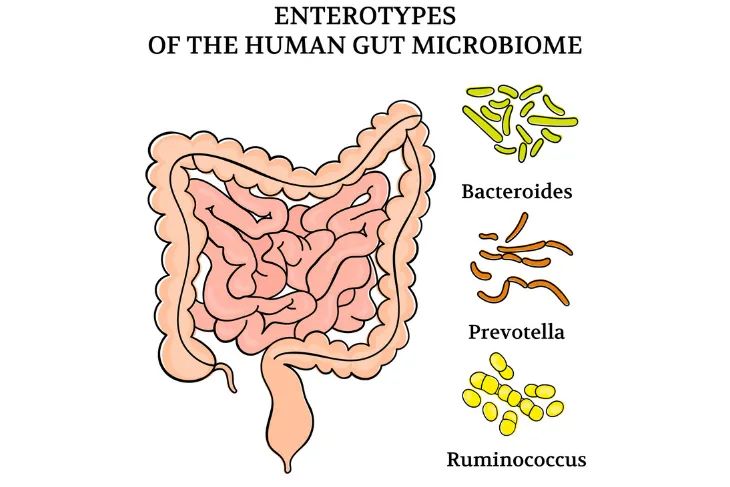
Medical experts who contribute to Medical Discovery News, a collaboration between Professor David W. Niesel and Professor Norbert K. Herzog, who met at the University of Texas, in Austin, claim that gut type is just as distinctive as a classifier blood type. For instance, the prevalent gut microbiome (or bacterial species in our intestinal tract) determines our individual “enterotype,” which begins colonizing the gut right after birth.
In total there are three different enterotypes—Enterotype 1 (characterized by a prevalent bacterium called Bacteroides, which produces greater rates of biotin or vitamin B7), Enterotype 2 (indicates increased capacity of bacterium, Prevotella, and produces greater levels of Thiamine or vitamin B1), and Enterotype 3 (while is largely distinguished by Ruminococcus bacterium).
Your Enterotype: Your Foundation for Health
You don’t have much of a choice when it comes to what enterotype you end up with. However, several things can affect your early balance of gut bacteria. For instance, vaginal delivery versus caesarean section birth, diet, home, antibiotic medications, intestinal infections, hygiene level, and living environment can all cause a shift in our individual gut bacteria.
And while a prevalence of certain gut microbiota may cause various health conditions—osteoporosis, Alzheimer’s, autism, and irritable bowel syndrome—the introduction of healthy (or good) bacteria via probiotic and prebiotic supplements and foods may positively aid digestion, immunity, and mood if gut flora balance is once again restored.
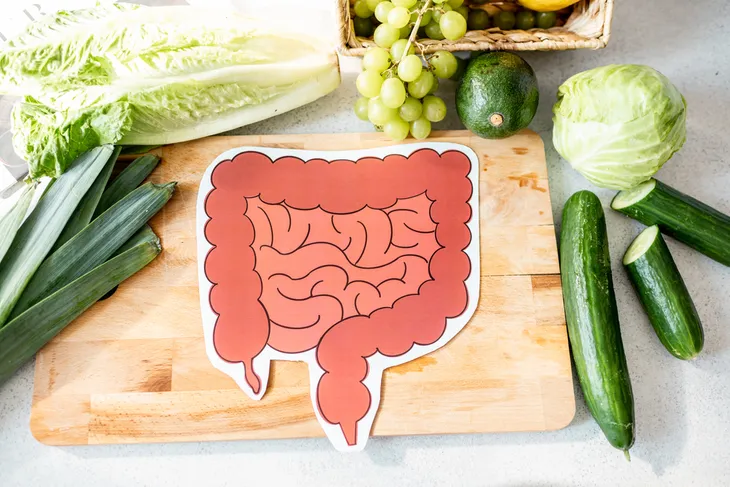
How Diet Influences Gut Health
When we eat we often consider our waistlines, blood sugar levels (if we’re diabetic), cholesterol (if we suffer from hypertension), and food allergies and intolerances. However, what you eat affects us at the base level, meaning it can affect that actual balance of gut itself.
This is why anatomists and biologists at Columbia University consider a healthy, well balanced diet (based on fresh fruits and vegetables, fibrous foods, lean proteins, and healthy fats) the best course of action rather than eliminating certain foods or eating from just certain food groups. Above all, listen to your gut: if a certain food disagrees with it, pay attention, your health may depend on it!
Get Gut-Friendly with Foods
You literally are what you eat if you consider all that stuff about enterotypes, and the fact that an overabundance of certain gut bacteria can lead to all sorts of health woes (i.e., depression, chronic inflammation, and type 2 diabetes). However, the introduction of gut-friendly bacteria (i.e., prebiotics) can also aid the immune system and minimize chronic health risks.
Biologists from North Carolina State University, caution us to be good to our guts by consuming an abundance of fibrous greens and veggies as well as prebiotic-rich foods (i.e., garlic, leeks, legumes, oats, asparagus, and bananas), and by getting frequent fresh air and regular exercise.
How the Gut is Linked to Metabolic Response
Researchers at Emory University, Atlanta, even link increased rates of obesity back to the gut. They believe that individual appetites are affected by a shift in dominant microorganisms in the gut, causing us to eat more, and in turn, gain weight.
For instance, if the gut flourishes with one dominant microorganism that triggers an inflammatory response, our cells may become immune to insulin and leptin—both crucial hormones that help regulate the rates that we store and use energy (or carbohydrates and fat). This may cause appetite to increase even though metabolism slows down.
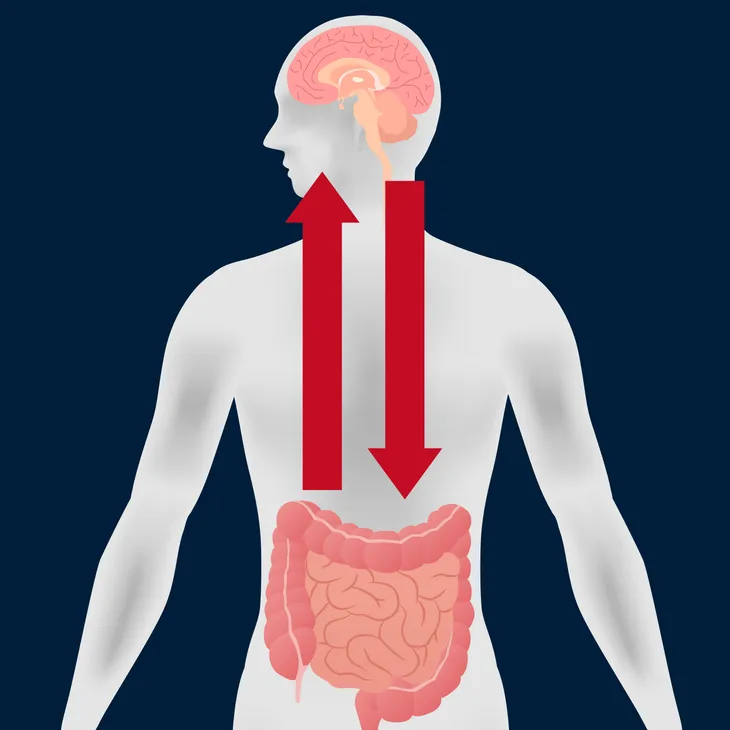
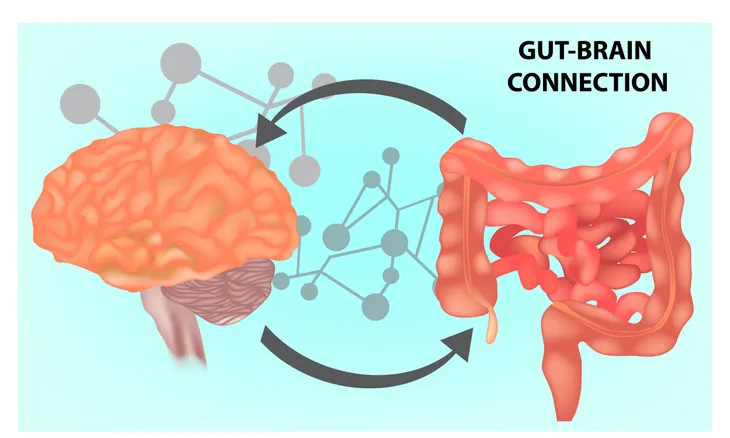
The Gut is the Body’s Second Brain
Many of us believe that our brains control our body and all of its systems and organs—including the digestive system. However, scientists now admit that the brain-gut connection isn’t lead by our brains as much as previously thought. Cell biologists at New York’s Columbia University claim the gastrointestinal tract acts as a second brain.
The gut contains an autonomous nervous system that not only functions independently (to control digestion) of the brain and spinal cord, but also encompasses hundreds of millions of neurons (equal to the spinal cord) and roughly 40 neurotransmitters (equal to the brain), which means approximately 95-percent of the vagus fibres carry signals from the gut to the brain as opposed to from the brain to the gut.
Gut Power Over Mood
There is little wonder that trouble in the gastrointestinal system affects mood. It turns out that the gut is home to 95-percent of our serotonin levels while the brain harbors a mere 2-percent of the happiness hormone. This is why gut woes can lead to depression, lower sex drive, insomnia, forgetfulness, and even loss of appetite.
Scientific research from John Hopkins University, in Baltimore, Maryland, even supports the claim that irritable bowel syndrome (or IBS) results in excessive serotonin levels in the gut, which also explains why so many with IBS also suffer from mood disorders (i.e., depression).