The knee is the largest joint in the body and knee pain is a common complaint across all age groups. It may be due to a diverse range of causes including sudden injury, overuse injury, or an underlying medical condition.
The location and severity of knee pain varies depending on the root cause. The thigh bone (femur) and lower leg bones (fibula and tibia) compose the knee joint. Structures found in or around the knee joint include discs (menisci), cartilage, ligaments, tendons, and muscles. Signs and symptoms that may accompany knee pain include swelling, stiffness, redness, warmth, weakness, instability, popping or crunching noises, fever, and decreased range of motion (inability to fully extend or flex the knee).
The 10 most common causes of knee pain are…
1. Patellofemoral Pain Syndrome
Patellofemoral pain syndrome, also known as runner’s knee, is a common cause of knee pain among runners. It can also strike those engaging in activities requiring repetitive knee bending such as biking, climbing, and jumping. Symptoms of this syndrome may include pain behind or around the kneecap (patella), pain while bending the knee, pain that worsens when walking downstairs or downhill, knee swelling, or popping or grinding sensations in the knee.
Patellofemoral pain syndrome can affect one or both knees. It can be caused by overuse (repetitive bending, high stress exercises, or overstretched tendons), direct trauma (fall or blow), misalignment of the kneecap or other leg bones, problems with the feet (hypermobility, fallen arches, or flat feet), and weakness in the thigh muscles or other muscle imbalance. Treatment of the syndrome may include rest, ice, compression, elevation, anti-inflammatory medications, stretching and strengthening exercises, and arch supports or shoe orthotics.
2. Chondromalacia Patella
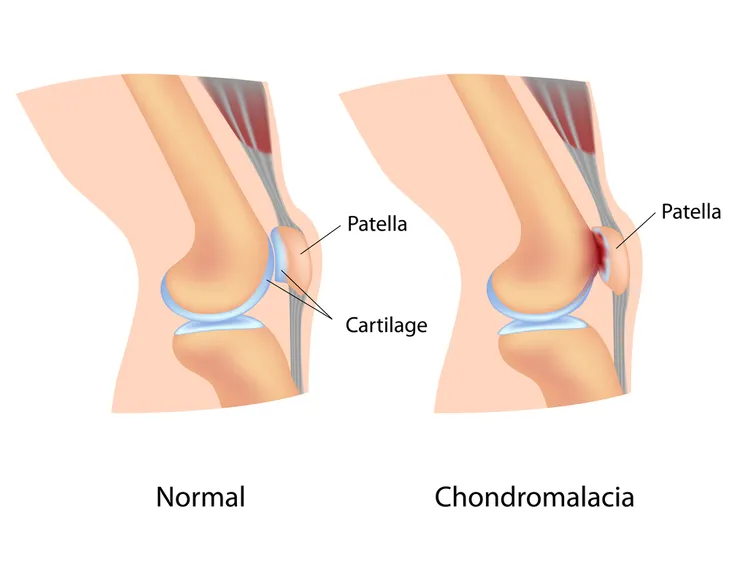
Chondromalacia patella refers to the softening and breakdown of the cartilage on the underside of the kneecap or patella. It is one of the common causes of knee pain, especially in women. Chondromalacia patella is caused by misalignment, or improper tracking, of the patella as it slides over the thigh bone (femur). The most common symptom is a dull, aching pain in the front of the knee behind the kneecap, which can be exacerbated by prolonged sitting.
Potential causes of the condition include muscle imbalances such as tightness in the iliotibial band and weakness in the quadriceps or hip rotator muscles. Physical therapy is a mainstay of treatment for chondromalacia patella and incorporates stretching and strengthening of the offending muscle imbalance, which most commonly occurs in the quadriceps muscle. Rest, ice, and anti-inflammatory medications may also be used to reduce inflammation and pain. The prognosis, or outlook for recovery, for chondromalacia patella is excellent.
3. Osgood-Schlatter Disease
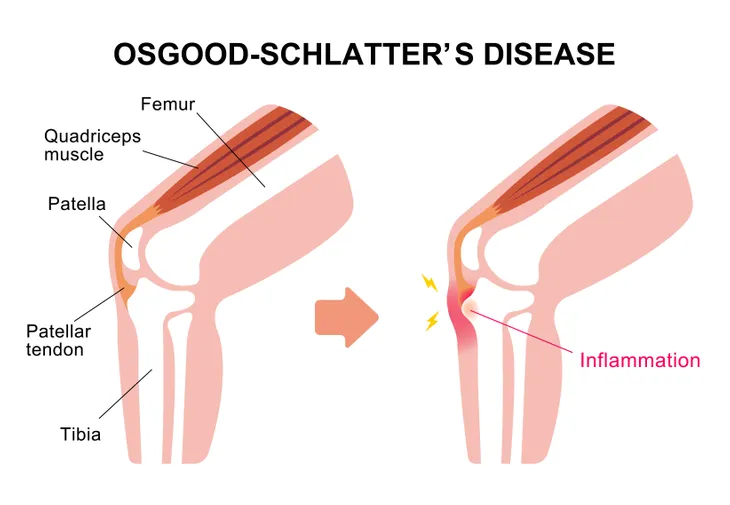
Osgood-Schlatter disease is a knee ailment most commonly diagnosed in children and adolescents. It can cause a painful lump below the kneecap (patella) in children and adolescents experiencing growth spurts. It most commonly affects children participating in sports such as soccer, basketball, volleyball, and ballet since they involve running, jumping, and swift changes in direction. The disease is more common in boys than girls. It can occur in one or both knees.
Repeated stress from running and jumping causes the tendon connecting the kneecap to the shinbone to pull away ending in pain and swelling. The resulting gap may be closed with new bone growth, which results in a bony lump below the kneecap. The pain of Osgood-Schlatter disease can vary from mild to chronic and debilitating. Anti-inflammatory medications and physical therapy may be help to decrease pain associated with the disease. Complications from the disease are uncommon. Osgood-Schlatter disease usually resolves after adolescence when bones stop growing.
4. Osteoarthritis
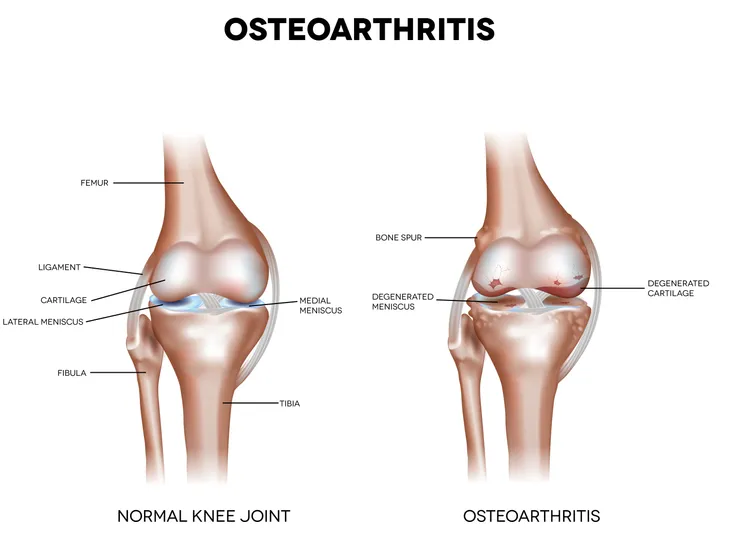
Knee osteoarthritis is a common medical condition. The United States Centers for Disease Control and Prevention (CDC) estimates the disorder affects more than 33-percent of individuals older than 65-years. It is a degenerative joint disease characterized by the deterioration of cartilage, overgrowth of bone at the margins (osteophytes), and increased bone density (subchondral sclerosis). Some common risk factors for the development of knee osteoarthritis include female sex, obesity, older age, and previous knee injury.
Most individuals suffering with knee osteoarthritis report pain that is worse with use and better with rest. Other signs and symptoms of the disease may include stiffness that generally improves after 30-minutes of activity, swelling, crepitus (a grating sound or sensation), and limp. Pain from the condition may be treated with topical agents like capsaicin cream (Zostrix); oral anti-inflammatory agents such as acetaminophen (Tylenol) or ibuprofen (Advil); and injections directly into the knee joint with agents such as steroids or hyaluronic acid (Synvisc). End-stage disease may have to be treated surgically with total knee replacement.
5. Bursitis
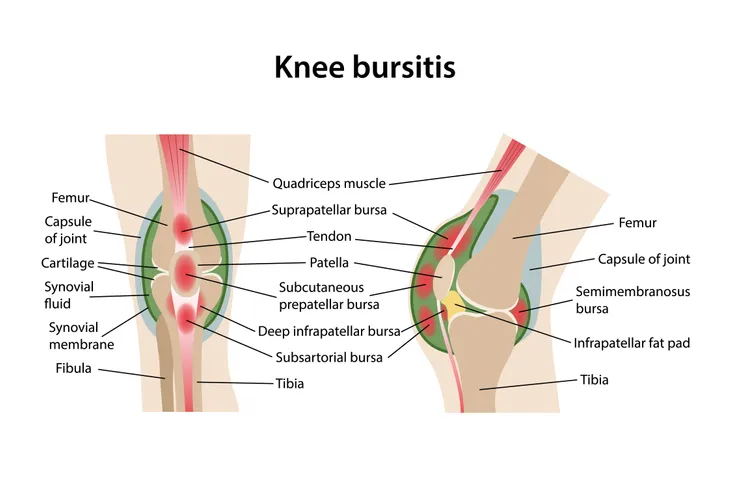
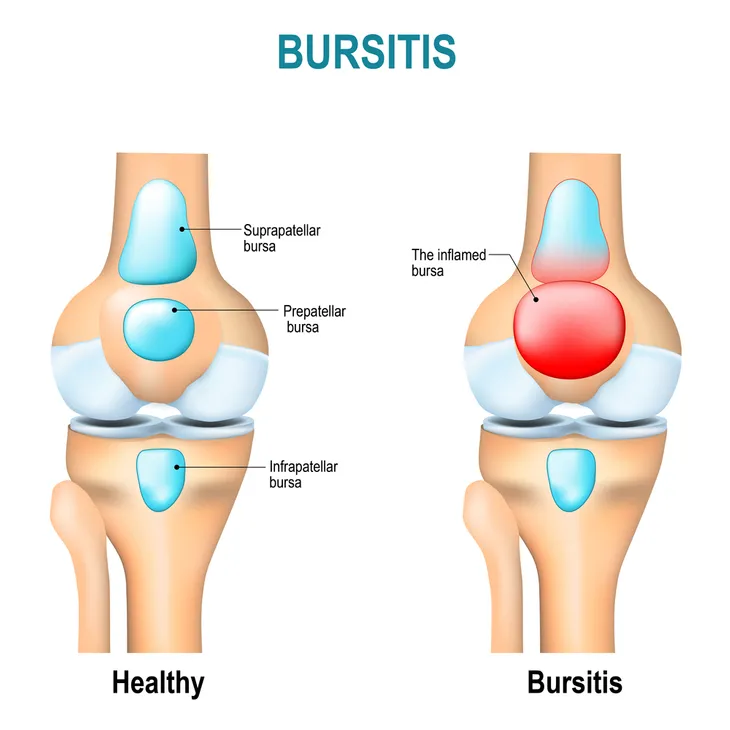
Bursitis of the knee refers to inflammation of a fluid filled sac (bursa) located near the knee joint. A bursa reduces friction and serves as a cushion to reduce pressure between bones and tendons and muscles near joints. Each knee joint has a total of 11-bursae. Causes of knee bursitis include frequent kneeling, a direct blow to the knee, bacterial infection of a bursa, and complications from other conditions such as osteoarthritis, rheumatoid arthritis, or gout in the knee.
Common symptoms of knee bursitis include pain, warmth, tenderness, and swelling of the affected bursa. Treatment of knee bursitis may entail the use of anti-inflammatory medications or antibiotics (if an infection is present). Other treatment modalities utilized for knee bursitis may include physical therapy, steroid injection, and aspiration (drainage) of the bursa. Surgery may be recommended for severe chronic bursitis unresponsive to other treatments. Prevention of knee bursitis may be accomplished by wearing knee pads, taking breaks from prolonged kneeling, and avoiding excessive squatting.
6. Popliteal Cyst
A popliteal cyst, or Baker’s cyst, represents an accumulation of fluid in the popliteal bursa, which is a small fluid-filled sac behind the knee. It is the most common cause of pain behind the knee. It is named for the British surgeon who first described the condition, Dr. William Baker. Popliteal cysts are usually caused by underlying medical conditions such as gout (increased levels of uric acid in the blood), hemophilia, lupus, osteoarthritis, psoriasis, rheumatoid arthritis, and injury.
Signs and symptoms of a popliteal cyst may include knee pain, swelling or lump behind the knee, calf pain, and clicking or locking of the knee joint. Treating the underlying cause of the Baker’s cyst usually causes resolution of the cyst. General measures used to treat a popliteal cyst may include rest, ice, anti-inflammatory medications, crutches, and compression bandages. Popliteal cysts that are particularly problematic may need treatment with steroid injection, physical therapy, or knee surgery.
7. Prepatellar Bursitis
Prepatellar bursitis refers to inflammation of the bursa (small fluid-filled sac) in front of the kneecap (patella). It is also known as housemaid’s knee. It not only affects housemaids, but also tradesmen such as roofers or carpet layers who repeatedly kneel. Prepatellar bursitis may be caused by sudden injury (fall or direct blow to knee), recurrent minor injury to the knee (repetitive kneeling), infection, gout, and rheumatoid arthritis. It can occur among individuals in any age group and is more common in males than females.
Symptoms of prepatellar bursitis may include pain in the front of the knee, redness and swelling in the front of the knee, and difficulty bending the knee, walking, and kneeling. Fever may accompany prepatellar bursitis caused by infection. Most cases of prepatellar bursitis respond to conservative treatment with rest, ice, anti-inflammatory drugs, and elevation of the affected knee. The condition may be prevented or kept from recurring with the use of knee pads.
8. Patellar Tendonitis
Patellar tendonitis is an overuse injury affecting the patellar tendon, which sits just below the patella (kneecap) and attaches the kneecap to the shinbone. It is also referred to as jumper’s knee. Activities requiring frequent jumping and landing place excessive stress on the patellar tendon. The stress results in tiny tears in the tendon. It commonly affects athletes involved in sports such as basketball, volleyball, soccer, football, track and field, tennis, gymnastics, and skiing. The condition can also be the result of aging.
Signs and symptoms of patellar tendonitis may include localized pain and tenderness over the patellar tendon, thickening of the patellar tendon, stiffness in the patellar tendon, and pain made worse by jumping, landing, or running. Patellar tendonitis usually responds well to conservative treatment such as rest, ice, anti-inflammatory drugs, stretching and strengthening of the quadriceps muscle, and physical therapy. Recovery from patellar tendonitis may take a few weeks to several months.
9. Iliotibial Band Syndrome
Iliotibial band syndrome (ITBS) occurs when the iliotibial band (the ligament that runs down the outside of the thigh from the hip to the shin) is tight or inflamed. It is one of the most common overuse injuries among runners. It can also be associated with activities such as cycling, hiking, or weight lifting. Iliotibial band syndrome is the most common cause of lateral, or side, knee pain. It is caused by excessive friction of the iliotibial band on the side of the knee.
The most common complaint of ITBS is diffuse pain over the lateral aspect (side) of the knee. Running, especially downhill, may aggravate the knee pain. Another common symptom of ITBS is weakness when moving the leg out sideways. Treatment options for the treatment of ITBS include rest, ice, anti-inflammatory medications, stretching and strengthening exercises, sports massage, and acupuncture.
10. Osteochondritis Dissecans
Osteochondritis dissecans (OCD) refers to a joint condition in which bone below the cartilage of a joint dies due to lack of blood flow. The dead bone and cartilage break loose causing pain and decreased joint movement. The condition can occur in any joint, but it most commonly affects the knee joint. Osteochondritis dissecans occurs most often in children and adolescents, especially those high active in sports. The exact cause of OCD is unknown, but scientists suspect it might result from repetitive trauma to bone over time.
Symptoms of osteochondritis dissecans affecting the knee joint may include pain, swelling, tenderness, joint popping or clicking, joint weakness, and decreased range of motion. Conservative measures such as rest and physical therapy are the mainstay of treatment for this disorder. Surgery may be needed for loose fragments in the knee joint or if conservative measures fail after 4 to 6-months.