Pelvic pain is no laughing matter. In fact, chronic pain in the nether regions has deterred women from tight pants, sexual intercourse, and even had them dredging the urge to urinate or even sit down.
Chronic pelvic pain is almost as difficult to diagnose because the discomfort can often indicate more than one health issue. However, being aware of the most common pelvic pain culprits—for example cysts and endometriosis—can ease worry and help catch the cause in its earlier stages.
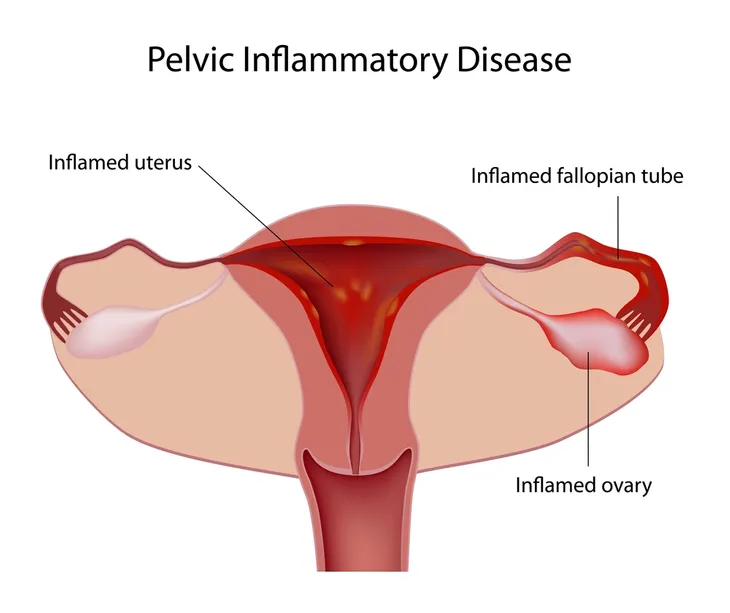
Pelvic Inflammatory Disease
PID strikes millions of American women each year. It may be caused by a sexually transmitted infection, such as chlamydia or gonorrhea, from sexual intercourse from a partner that spreads into the pelvis. PID can also be contracted following childbirth, an abortion, or a pelvic procedure if bacteria enter the cervix and migrate upwards to the uterus, cervix, and/or fallopian tubes.
PID cases can be treated effectively if it’s caught early on. That’s why it’s important to be on guard for symptoms of abdominal pain, chills, vaginal discharge, rapid heart rate, and back pain.
Endometriosis
Approximately 5 million women in the U.S. suffer with endometriosis, a chronic condition in which uterine lining cells grow and spread outside the uterus and painfully break down when the uterine lining is shed during your monthly menstrual period.
The symptoms of endometriosis include painful abdominal cramps as well as pain in the lower back and legs.
Pelvic Congestion Syndrome
Ever feel weighed down—in your pelvic floor? If you do, you may be the unlucky recipient of pelvic congestion syndrome, a condition that encourages the formation of varicose veins in the pelvis, which results in painful blood pooling and severe pelvic pressure.
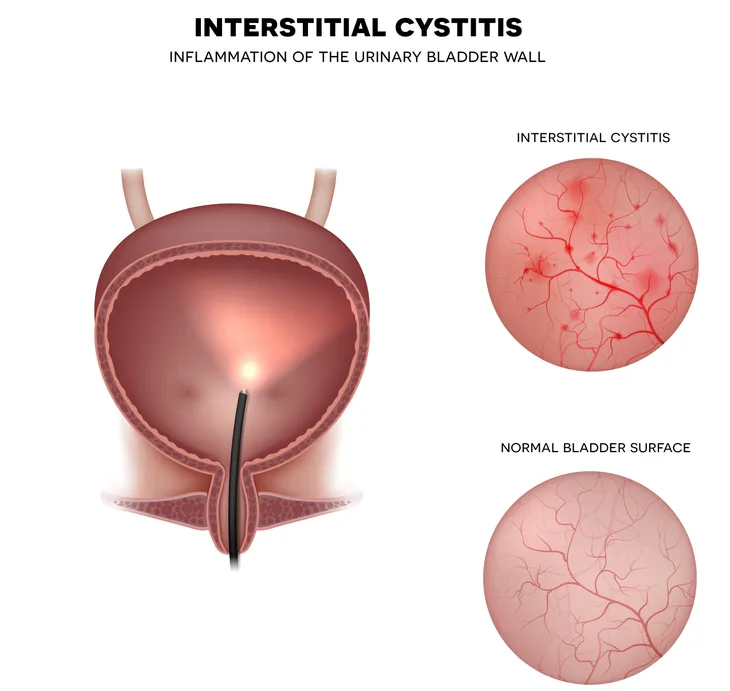
Interstitial Cystitis
Interstitial cystitis affects between 3 and 8 million women in the U.S. causing symptoms of bladder pain. This pain is often described as burning or a stabbing pain that rears its ugly head as if you have the worst urinary tract infection—on earth!
The condition is caused when mucin, the protective cells protecting the bladder from acid, wear down, causing the painful need to urinate up to 50 times per day.
Bacterial Vaginosis
The most common chronic vaginal infection among women of childbearing age, bacterial vaginosis (or BV) strikes about 16-percent of all women with symptoms of itchy or burning sensations around the outside of the vagina as well as a foul, fishing-smelling, grayish discharge that can be mistaken for a yeast infection.
Pelvic Floor Tension Myalgia
A strenuous vaginal childbirth can cause a condition called pelvic floor tension myalgia, or chronic tension in the muscles of the pelvic floor. If that doesn’t have you practicing your Kegal exercises (a series of contractions and relaxation techniques to align the muscles of the pelvic floor), the weighted feeling (a pelvic heaviness or ache) and pain in the vagina might prompt a visit to a medical professional.
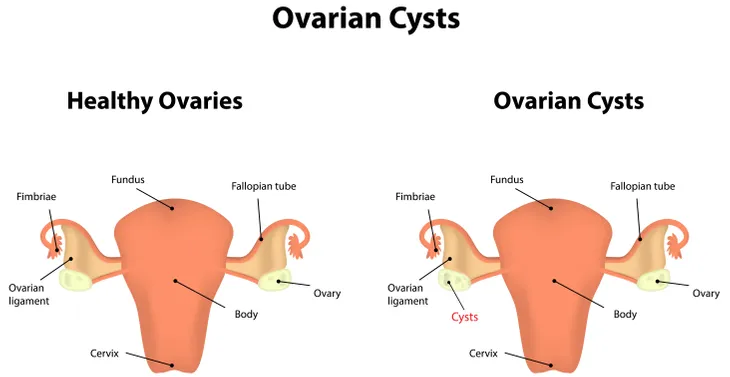
Ovarian Cysts
Mainly a torment to women of childbearing age, ovarian cysts are blister-like, fluid-filled sacs that develop on the ovaries. Most often harmless in nature, these cysts will rupture each time an egg is released during ovulation.
Ovarian cysts are often painless, however, during or following intercourse a woman may feel a dull ache, sharp pains, or feel pressure in the abdominal area.
Vuvodynia
If you’re vagina’s depressed, you’re not alone. More than 6 million women suffer from a sad vag-jay-jay—aka vulvodynia—or chronic vulvar pain. A condition thought to be spurred by a series of yeast infections, sexual encounter, or a difficult child-birthing experience, vulvodynia results in a persistent burning pain at the vaginal entry, upper thighs, and buttocks.