Polycystic ovary syndrome is a hormonal condition that is actually quite common. It causes the overproduction of androgens (or male hormones) in women which then causes havoc in the female body—messing with the menstrual cycle (causing irregular periods), causing the development of small unruptured follicles in the ovaries, impacting cardiovascular health, causing hair and skin issues, and making it rather difficult to conceive (as androgen levels affect ovulation and egg release).
This condition is uncomfortable for women due to the array of symptoms that come with it, but it’s particularly frustrating for women who are trying to conceive. To raise awareness and understanding about this condition, here are some quick but important facts about PCOS…
It’s a Hormonal Disorder
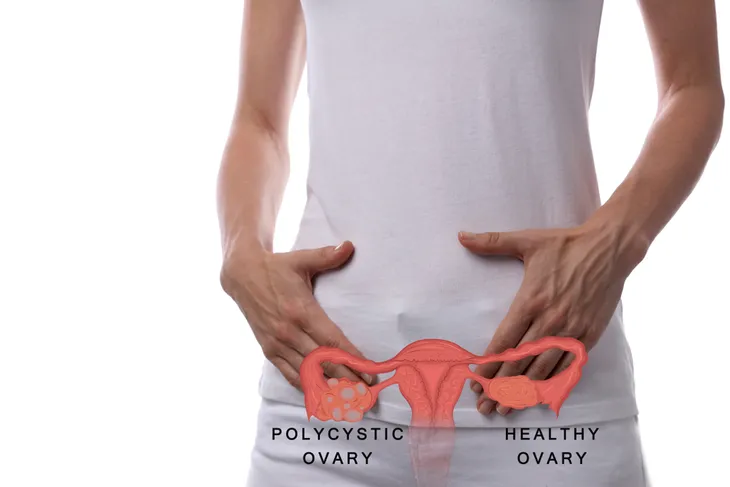
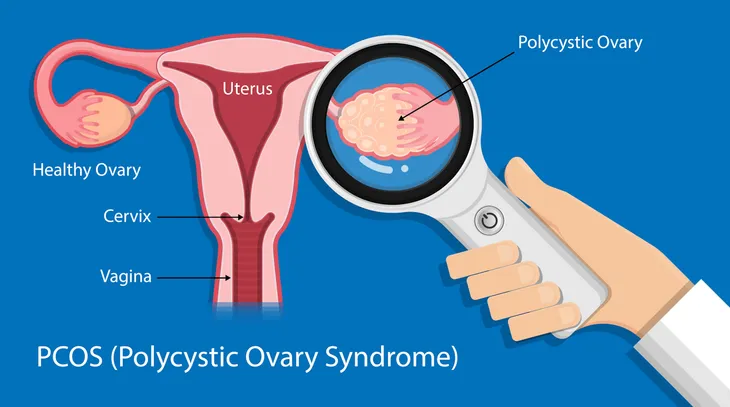
We tend to associate hormones with women, but there are “male” hormones too. These hormones are called androgens and believe it or not, our ovaries produce them! Women with PCOS have ovaries that produce too many androgens which causes missed periods, body hair, hair growth, weight gain, and acne. This excess of androgen can cause problems around ovulation and fertility. “Each cycle, a follicle is supposed to break open and release a mature egg. In women with PCOS, that doesn’t happen. Instead, the follicle sticks around as a tiny cyst,” explains Prevention.
According to Jessica Lalley, MD, a board-certified ob-gyn and associate clinical professor at Michigan State University, it’s still unclear whether the cysts are what is producing this excess androgen or they are a result of it. “It’s a chicken-or-egg thing,” says Lalley to Prevention.
How Many Women Are Affected by PCOS?
According to the U.S. Department of Health and Human Services, between five and 10-percent of women in their childbearing years and one in 10 women as young as 11-years of age are affected by PCOS—with an estimate total of 5 million women in the U.S. affected overall. Unfortunately, even though PCOS is so common and widespread, it’s still extremely misunderstood and is often misdiagnosed or undetected. So women need to be their own advocate and do their own research in order to get in front of their own fertility and health.
“PCOS is one of the most critical, underserved, under-diagnosed and under-funded conditions affecting women’s health. We need the help of media, government agencies and funding sources to improve patient outcomes and help save lives,” says Sasha Ottey, founder and executive director of PCOS Challenge Inc., to Huffington Post. If you suspect you are suffering from PCOS or have been diagnosed with it, Amy Medling, certified health coach and founder of pCOS Diva, suggests educating and empowering yourself.
What Causes PCOS?
Although the exact cause of PCOS is still unknown, medical experts have a few theories…
First up, researchers have linked high [the hormone that regulates the amount of glucose in the blood] levels to an increased incidence of PCOS in women—meaning that high levels of the hormone that breaks down sugars and starches into energy has been shown to also increase the levels of androgen production. Excess androgen is another potential cause. The Mayo Clinic points out that if the ovaries produce too much androgen this could result in hirsutism and acne.
Medical experts also believe that genetics may be a factor—as a high rate of PCOS patients have a blood relative with the condition (i.e., sister or mother). This might be helpful for diagnosing the condition which is typically difficult to diagnose. Another cause is low-grade inflammation. “This term is used to describe white blood cells production of substances to fight infection,” writes the Mayo Clinic. “Research has shown that women with PCOS have a type of low-grade inflammation that stimulates polycystic ovaries to produce androgens, which can lead to heart and blood vessel problems.”
Fertility Issues
Although the symptoms of PCOS vary from woman to woman, the majority of sufferers are stricken with fertility difficulties and menstrual irregularities. Both can be explained by the overproduction of androgen hormones and the limited production of progesterone hormone needed for ovulation and egg production, as well as by cysts (or fluid filled sacs) that form on the ovaries and impede progesterone production. “If you don’t get a period every month, then you’re not ovulating every month,” says Anuja Dokras, MD, PhD, director of Penn Medicine’s Polycystic Ovary Syndrome Center and President of the Androgen Excess and PCOS Society to Prevention. “So the chances of getting pregnant go down. You may need help from a fertility doctor or ob-gyn.”
Although PCOS is the most common cause of infertility in women, it’s not a lost cause. Many women with this condition go on to have children, it’s just a little more difficult to get there. Women with PCOS still have healthy eggs, it just means you might need to work with an ob-gyn to get your cycle regulated. Huffington Post refers to research by Penn State College of Medicine which found that the drug letrozole helped improve birth rates among women with PCOS.
Symptom: Irregular Hair Growth
In addition to struggling with scary menstrual and fertility issues, PCOS can also cause a collection of hormone-related symptoms that may make women feel as if they have zero control over their bodies. As mentioned, PCOS symptoms vary between women, however, irregular hair growth is one of the more commonly shared symptoms. And by irregular, I mean totally confounding! On the one hand PCOS can cause thinning hair (or male pattern baldness), but on the other hand it can also trigger excess hair growth (a condition referred to as Hirsutism) on areas uncommon and embarrassing to women—including the face, toes, back, chest, stomach, and fingers.
Again, not every woman will experience this symptom. “Ethnicity may predispose a patient to having excess hair,” says Loren Wissner Greene, MD, professor of endocrinology and ob-gyn at NYU Langone Health to Everyday Health.
Symptom: Skin Problems
PCOS can wreak havoc on the appearance of female patients with a series of exterior and rather embarrassing skin issues. Many women develop patches of dark brown or even black, thick skin on their arms, necks, thighs, and breasts. Sudden outbreaks of acne are also common on the face, back, and neck. In addition to all this, skin tags, which develop as small, excess flaps of skin can also appear on the neck and under the armpits.
Symptom: Pain
Many women who suffer from polycystic ovary syndrome also complain of severe pelvic pain among their many symptoms. The pain is often characterized as throbbing, recurrent pain on one or both sides of the pelvis, in the area of the ovaries that worsens during and around menstruation. Medical experts speculate that the pain may be caused by inflammation in the ovaries or heavy or prolonged periods.
Symptom: Gloomy Mood
Medical experts often debate over the issue of whether depression and anxiety are side effects of the hormonal imbalances that PCOS causes—or if mood changes are the result of dealing with the many symptoms of PCOS (i.e., irregular hair growth, skin issues, baldness, weight gain and more). However, a study from the Department of Medicine at University of Chicago Hospital found that increased free testosterone (FT) levels in PCOS patients may be the prime cause of mood-related disorders as heightened FT levels are linked to depression, anxiety, and negative mood.
Symptom: Difficulty Losing Weight
As if women didn’t have enough trouble losing weight this condition makes it even harder! While it’s harder, it’s not impossible. Many women have had successful losing weight while struggling with this condition. Plus, an added bonus is that weight loss can help alleviate the symptoms. Typically weight loss is dependent on how many calories a person is eating in a day versus how many calories they are burning through things like exercise. However, for those with PCOS it might not be that simple.
“We know now that weight loss is more complicated. For example, the gut flora may be different in women with PCOS, which can play a role in metabolism,” says David A. Ehrmann, MD, director of the University of Chicago Center for PCOS in Illinois to Everyday Health. So don’t worry, it’s not in your head! As with fertility, it’s not impossible, but it just means it’s going to be a little bit harder.
Even Good Doctors Can Miss It
As we mentioned earlier, PCOS is actually quite common, but a lot of women don’t even realize they have it until they start trying to conceive. One of the reasons it’s so often misdiagnosed or goes undetected is because there is no test that can be used to distinctively determine whether a woman has PCOS or not. There are also a lot of factors that differ between women. Nearly 80-percent of women with PCOS are obese, but that also leaves a good chunk of women who aren’t. Also, many of women with PCOS have small cysts on their ovaries, but not all. It’s not a condition that has a “one size fits all,” says Huffington Post. The source also notes that this is why less than 50-percent of women are properly diagnosed.
According to Prevention, the way doctors typically diagnose PCOS is through “diagnosis of exclusion” which basically means they will rule out other conditions that can mimic it. What makes it even more complicated is that the symptoms are all over the place and often treated by different medical specialists. For example the acne that is caused by PCOS is often treated by a dermatologist who then might not ask about your irregular periods, and a gynaecologist might know about irregular periods, but not realize that you also have unusual body hair growth.
Weight Loss for Treatment
There’s this misconception around PCOS that only overweight or obese women struggle with it. This isn’t true. While it definitely puts someone at a higher risk for having PCOS, there are many women who aren’t struggling with their weight who also have this condition. That being said, for the most part has shown to help alleviate symptoms. Prevention explains that the theory is that obesity “contributes to [the hormone that regulates the amount of glucose in the blood] resistance, which boosts androgen levels and can make PCOS symptoms worse.”
As a result, losing weight can help with the problem. “Even losing 5-percent of body weight will have an impact on a woman’s whole metabolic profile,” says Jessica Lalley, MD, a board-certified ob-gyn and associate clinical professor at Michigan State University to Prevention. That’s not a whole lot to lose, especially if it can help with trying to conceive. Unfortunately, as we already mentioned, losing weight can be harder for women with PCOS.
Women who aren’t trying to conceive but want to alleviate their symptoms should consider taking an oral contraceptive to relieve symptoms and regulate their hormones and menstrual cycle.
Does it Go Away During Menopause?
This one is tricky because it can be the case, but isn’t always. Since PCOS affects many aspects of the body it depends. “Many women with PCOS find that their menstrual cycles become more regular as they get closer to menopause,” writes the U.S. Department of Health & Human Services. “However, their PCOS hormonal imbalance does not change with age, so they may continue to have symptoms of PCOS.”
In addition to all this, the source points out that a woman’s risk for diabetes, stroke and heart attack all increase as they age which means the PCOS health-related risks increase. We’ll get into more detail on what these risks are in the next slide.
Linked to Other Health Conditions
As if having polycystic ovary syndrome on it’s own wasn’t bad enough, this condition is also linked to together health problems like diabetes, high blood pressure, unhealthy cholesterol, sleep apnea, depression and anxiety, as well as endometrial cancer, says the U.S. Department of Health & Human Services.
When it comes to diabetes, the source notes that more than half of women with PCOS will have diabetes or prediabetes. Women with PCOS are also at a greater risk for high blood pressure compared to those who are the same age and don’t have PCOS. When it comes to cholesterol, “women with PCOS often have higher levels of LDL (bad) cholesterol and low levels of HDL (good) cholesterol,” writes the Office on Women’s Health. Both high cholesterol and blood pressure put them at an additional risk for heart disease and stroke.
Obstructed sleep apnea (OSA), or intermittent stalled breathing during sleep, is common to PCOS patients. According to a U.S. Institutes of Health sleep study that monitored 505 women (53 women with PCOS, between the ages of 16- and 45-years-old, and a control group of 452 women, ranging in age from 20- to 42-years-old). Findings showed a 30-percent prevalence of OSA and sleep disordered breathing (or SDB) in PCOS patients compared to the control group. Luckily, PCOS-related sleep apnea can be managed by seeking medical treatment, and by making healthy diet and exercise changes.
Lastly, “problems with ovulation, obesity, [glucose regulation] resistance, and diabetes (all common in women with PCOS) increase the risk of developing cancer of the endometrium (lining of the uterus or womb),” says the source.
Diagnosis
We already briefly talked about this, but what makes PCOS so hard to diagnosis is that there is no definitive way to do it. It requires a trip to the doctor who will then ask questions about your menstrual cycle and weight changes. Your doctor will need to do a physical exam checking for unusual hair growth, acne, etc. Other exams that might be involved are a pelvic exam which involves a visual and manual inspection of reproductive organs. There could also be a blood test to measure hormone levels or/and an ultrasound where the doctor checks the appearance of the ovaries and the thickness of the uterus lining, says Mayo Clinic.
If you are later diagnosed with PCOS then you might need to have additional tests done including periodic checks of blood pressure, glucose tolerance, as well as cholesterol and triglyceride levels. You might undergo screening for anxiety and depression as well as sleep apnea.
Treatment Options
Although there is no known cure for PCOS, there are treatments to help manage and soothe the symptoms of the condition. For instance, patients can talk to their doctor about sleep difficulties, prescription birth control can help manage irregular periods, and androgen-blocking and insulin-sensitizing medication is often prescribed to help control hair growth and loss, soothe skin issues, regulate ovulation, and improve fertility chances.
There are also a number of things that patients can do to limit their risk of long-term health problems like diabetes and heart disease. The best thing to do for this condition is to eat healthy and exercise regularly. As we already mentioned, many women with PCOS are overweight or obese, so managing weight could go a long way in terms of relieving their symptoms.
For women who are struggling to get pregnant, WebMD explains that a doctor would prescribe medication to help get you pregnant. “Letrozole encourages steps in the process that trigger ovulation. If they don’t work, you can try shots of hormones called gonadotropins,” writes the source. Lastly, there is in vitro fertilization (IVF). This process has the “egg fertilized outside of your body and then placed back inside your uterus. This may be the best way to get pregnant when you have PCOS, but it can get expensive.”