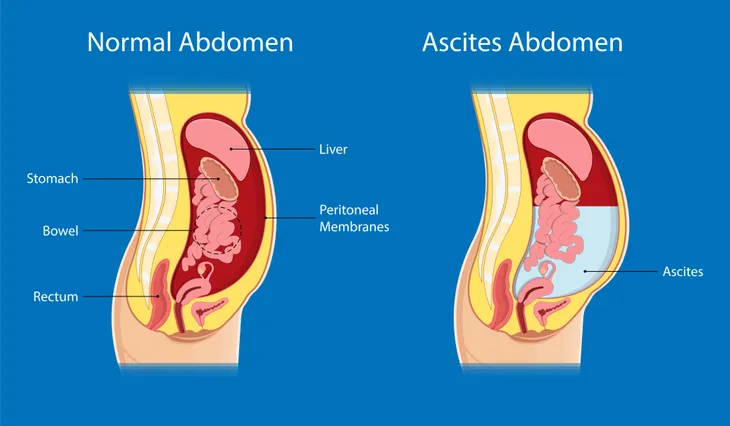
Ascites occurs when there is an abnormal buildup of fluid inside the abdominal cavity (“the belly”). Healthline notes an abnormal amount of fluid is anything more than 25-milliliters. It’s often the symptom of another cause, such as cirrhosis (scarring of the liver) and usually occurs when the liver begins to fail. Other causes include cancer and heart failure.
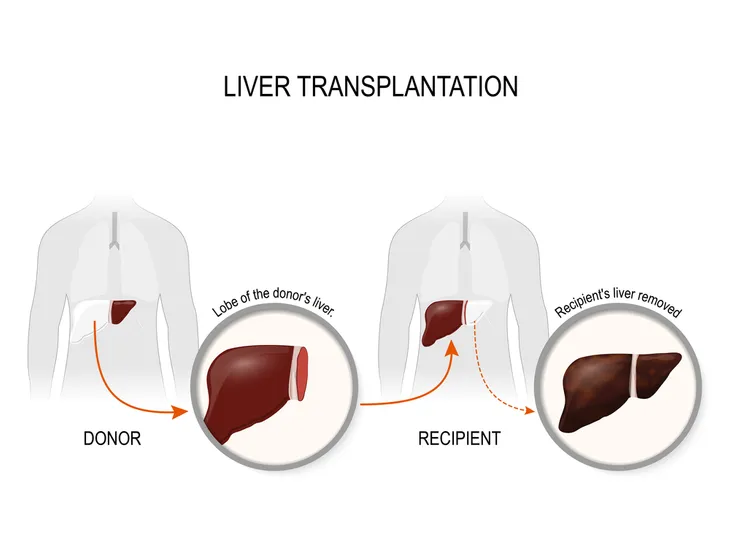
It is a serious health risk that develops when the liver is not working properly. When the liver stops working, “fluid fills the space between the abdominal lining and the organs,” writes Healthline. This is often the case in advanced liver disease, which means patients should be referred to a specialist for a potential liver transplant. The survival rate after ascites develops is 30- to 40-percent.
If you suspect you have ascites, talk to a doctor immediately. In the meantime, here’s more information on the condition and everything to know about ascites.
What is Ascites?
Ascites is the result of abnormal fluid buildup in the abdomen, and according to WebMD, is often caused by liver disease. Whenever there is fluid buildup in the body, it results in swelling, which is exactly what happens with ascites. The belly will become swollen and distended.
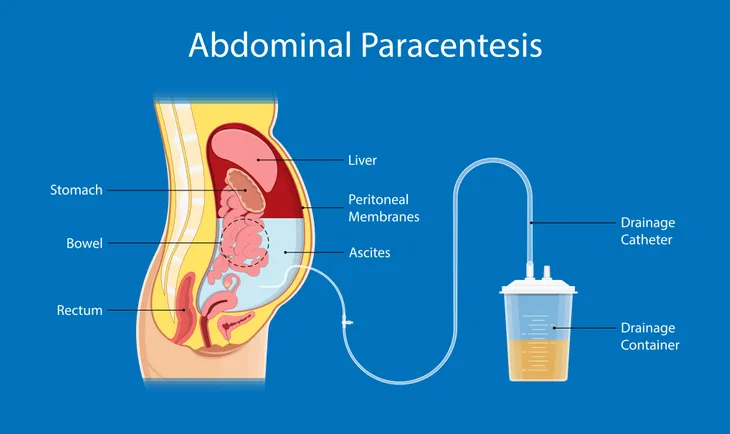
“This buildup occurs between two membrane layers that together make up the peritoneum, a smooth sac that contains the body’s organs,” explains Medical News Today.
Symptoms
Symptoms of ascites can appear suddenly or slowly over time. According to Medical News Today, it often develops over a few weeks, but it can also happen in just a couple days. It all depends on the cause of the fluid buildup.
Due to swelling and the ballooning of the belly, people with ascites often report a feeling of “fullness” in their abdomen. Another related symptom is weight gain. You may also experience shortness of breath, nausea, swelling in the legs and ankles, indigestion, vomiting, heartburn, loss of appetite, fever, and hernia. If you have any number of these symptoms, please see your primary care doctor immediately.
Not surprisingly, there’s also a lot of discomfort with ascites. This fluid retention puts pressure on internal organs, which can lead to abdominal and back pain, as well as difficulty breathing or even moving.
Causes
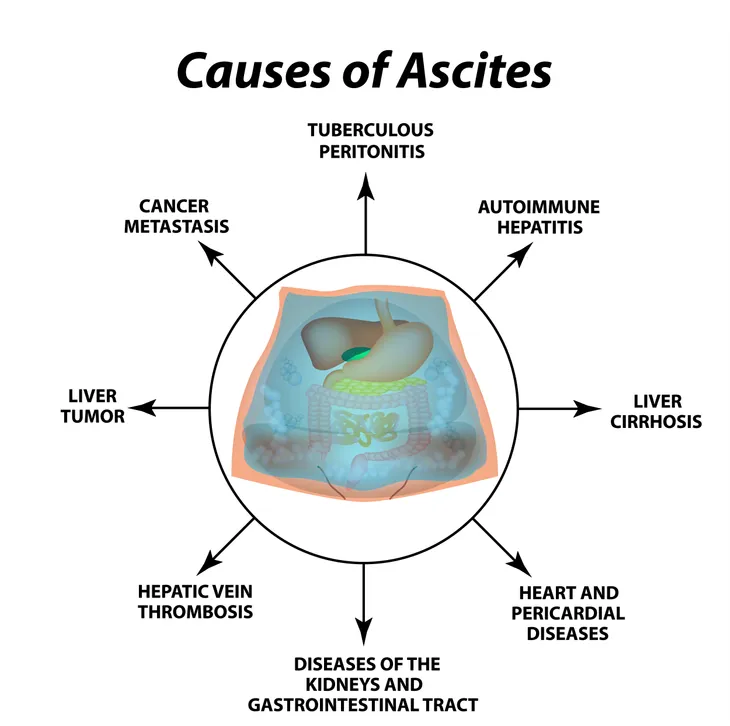
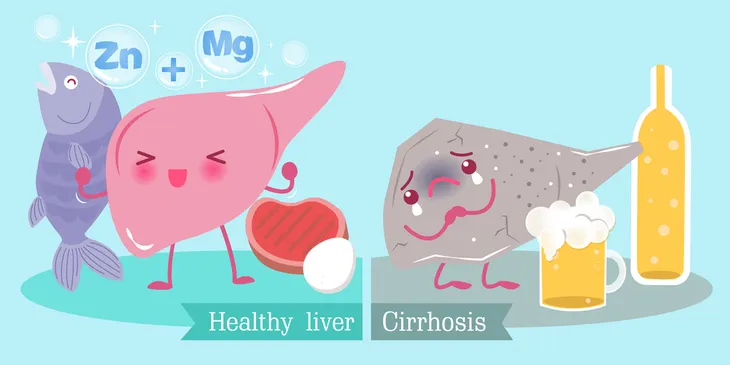
Ascites is often the result of pressure building up in the veins of the liver, which then causes them to not work properly. This increased pressure forces the buildup of fluid in the abdominal cavity. This is often the result of other conditions, such as cirrhosis, heart or kidney failure, or infection.
“The pressure blocks blood flow in the liver. Over time this keeps your kidneys from removing excess salt from your body. This, in turn, causes fluid to build up,” writes WebMD.
Risk Factors
According to WebMD, anyone with liver damage or scarring is at risk for ascites. These are the biggest risk factors. Other risk factors are viral infections, such as hepatitis B or hepatitis C, alcohol abuse, cancer in the organs (particularly the abdominal area), kidney failure, and congestive heart failure.
Healthline also includes ovarian, pancreatic, liver or endometrial cancer, pancreatitis, tuberculosis, and hypothyroidism. The prognosis of ascites depends on the underlying cause.
Complications
Ascites is a serious condition that can result in further complications. These complications include abdominal pain and pleural effusions (“water on the lung”) that can cause difficulty breathing. You may also suffer from a groin hernia (inguinal hernia), bacterial infection (spontaneous bacterial peritonitis [SBP]), or hepatorenal syndrome (which is a rare type of progressive kidney failure), says Healthline.
Infection
One of the main complications associated with ascites is infection. The fluid that is building up in the gut can become infected with bacteria. The result is a condition called bacterial peritonitis, according to Cleveland Clinic. The symptoms associated with this condition are abdominal pain and fever.
A doctor may diagnose this condition by taking a small sample of the abdominal fluid through a procedure called paracentesis which removes fluid from the abdomen using a long, thin needle. “Spontaneous bacterial peritonitis is a serious condition that requires treatment with IV antibiotics,” writes the source. “After recovery from this infection, long-term treatment with oral antibiotics is needed to keep the infection from recurring.”
Fluid in the Lungs
When fluid builds in the lungs (a condition referred to clinically as a pleural effusion) of an individual with cirrhosis, it’s called hepatic hydrothorax, says Cleveland Clinic. The fluid build up from the abdomen enters the lungs (mostly on the right side) and results in shortness of breath, coughing, hypoxia (lack of oxygen in the blood), and/or chest discomfort. This condition is best treated by paracentesis.
Kidney Failure
Ascites is often caused by cirrhosis of the liver which can lead to kidney failure if it continues to get worse. If this happens, it can lead to a condition called hepatorenal syndrome. It is extremely rare but must be taken seriously as it can lead to kidney failure.
Diagnosis
If you suspect you have ascites, you should go see your doctor immediately. Your doctor will perform a physical exam to check for any swelling in the abdomen and ask about your symptoms. In order to diagnose ascites, they may also perform a variety of blood tests, an ultrasound, or a computed tomography (CT) scan to look for fluid. Other testing methods may include magnetic resonance imaging (MRI), laparoscopy, or an angiography.
If your doctor determines you have ascites, there are a number of treatment options available. According to WebMD, they will likely perform a procedure called paracentesis (which uses a needle to remove fluid from your belly) in order to determine what is causing your ascites. You may also be referred to a liver specialist.
Treatment Options
Reduce Salt Intake
The American College of Gastroenterology says the most important step to take when someone is diagnosed with ascites is to reduce their salt intake to 4- to 5-grams per day (2,000-mg of sodium) or less. Because there is so much hidden salt in our food, it’s often recommended that patients work with a nutritionist to learn about the various foods they should avoid.
“Patients may use a salt substitute, but it is essential to choose one without potassium because the potassium levels can increase with certain medications to treat ascites,” writes the source. You will need to discuss with your doctor or dietitian what, if any, salt substitutes are safe for you to use. (Please see Diet and Lifestyle Tips for Liver Disease Patients).
Diuretics
This is the most common and effective form of treatment for ascites. Diuretics are sometimes referred to as “water pills” and are used to help flush any extra fluid out of the body, reducing any pressure in the veins around the liver. The two most commonly used diuretics are furosemide (Lasix) and spironolactone (Aldactone), says WebMD. Both of these help remove sodium and water from the body.
Anyone who’s taking diuretics will likely have to have their blood monitored by a doctor. You’ll also need to reduce your alcohol and salt intake.
Other Treatment Options
If diuretics and a change in diet don’t help, there are more aggressive forms of treatment available. These are often used in more serious or severe cases of ascites.
Paracentesis
If your case is resistant, a doctor may use paracentesis as a management technique. This procedure involves removing large amounts of fluid from the body with a long, thin needle that is inserted through the skin, and into the abdominal cavity. The goal is to reduce pressure and any discomfort. “In some instances, a person’s abdomen might contain about 5-liters of fluid, but in some extreme cases of ascites, doctors have drained more than 10-liters of fluid from the abdomen,” says Medical News Today.
This procedure does carry some risk of infection, so you’ll likely be prescribed antibiotics. Anyone who has this treatment must then follow a very strict low-salt, low-liquid diet afterwards, otherwise the fluid buildup will return, explains WebMD. Paracentesis is only used in cases when ascites is severe, recurrent, or when other treatments such as diuretics won’t work (i.e., late-stage cases).
Surgery
Surgery is often a last resort if all other options fail and is often reserved for extreme cases. During surgery, your doctor will place a shunt (a permanent tube) in the liver to reroute blood flow. “By increasing blood flow, all organs of the body are better able to perform their function,” writes Cleveland Clinic. “For example, in patients with ascites, improved kidney function helps rid the body of excess sodium (salt) and prevent the buildup of fluids.”
Another option is to replace the liver altogether with a liver transplant. However, this is another last resort option and only used for end-stage liver disease.
How to Manage Ascites
If you’re diagnosed with ascites it’s important to start weighing yourself daily. Any unusual weight gain could be a sign of fluid retention. The Cleveland Clinic warns that if you gain more than 10-lbs (or 2-lbs per day, 3 days in a row), you should call your doctor immediately.
To manage this condition, it’s extremely important that you cease or limit your alcohol intake. This can help reduce the risk of ascites developing in the first place and prevent it from getting any worse. You should also limit the use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, aspirin, indomethacin, or sulindac. “These drugs affect the kidneys, causing water and salt to be retained by the body,” writes the source.
Lastly, you should limit your sodium intake to no more than 2,000-mg per day.