- Vasculitis is the inflammation of the body’s blood vessels.
- Symptoms will vary depending on which blood vessels are affected.
- If organs are affected you may experience additional symptoms.
- Some types of vasculitis can worsen quickly so early intervention is key!
Actor Ashton Kutcher, 44, recently opened up about having a rare form of vasculitis that he said “knocked out” his vision, hearing, and equilibrium. The former That ’70s show actor said it took him nearly a year to recover and that he’s lucky to be alive. Developing a rare autoimmune disorder can be frightening for anyone so it’s best to get informed. So, what is it exactly?
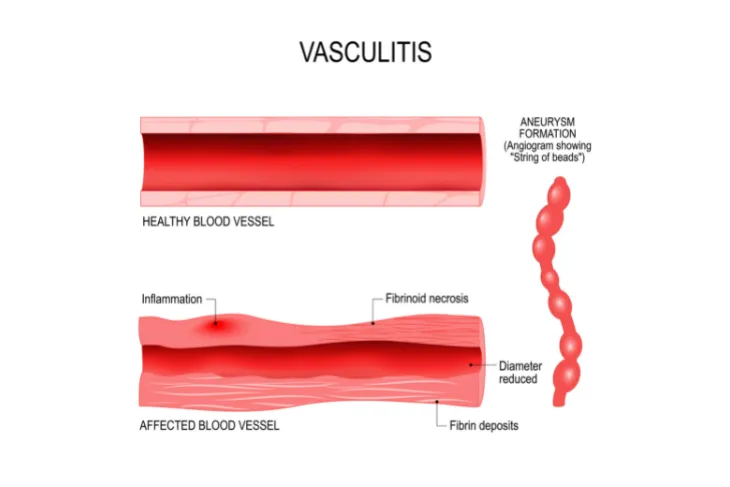
Vasculitis involves inflammation of the blood vessels which can cause the walls of your blood vessels to thicken and in turn, reduce the width of the passageway through the vessel, explains the Mayo Clinic. To make it even more complicated, there are many types of vasculitis, each affect the body differently. Luckily, most types are rare.
Follow along as we look into what vasculitis is, the different types, and signs that you may have it. We’ll also dive into what causes vasculitis, how it’s treated, and find out if it’s preventable.
What Is Vasculitis?
In short, vasculitis is the inflammation of the body’s blood vessels. Vasculitis can affect all sizes of blood vessels from very small (capillaries) to large blood vessels like the aorta.
“When inflamed, the blood vessels may become weakened and stretch in size, which can lead to aneurysms,” explains the Cleveland Clinic. Vasculitis can also cause the vessels to become so thin that they rupture which causes bleeding in the tissue. In some cases, it can cause the blood vessel to narrow and may even close it off completely (known as occlusion). This may lead to organ damage and it can even be life-threatening.
Common Signs and Symptoms of Vasculitis
The signs and symptoms will vary depending on which blood vessels are affected. If any organs are damaged you may experience additional symptoms. That said, Medical News Today says most cases of vasculitis typically involve the following symptoms:
- fever
- fatigue
- loss of appetite and weight loss
- joint pain
- muscle pain
- weakness and numbness.
These symptoms can mimic many other illnesses so it’s important to contact your doctor for a proper diagnosis.
 Prostock-studio / Shutterstock
Prostock-studio / ShutterstockTypes and Causes of Vasculitis
Unfortunately, the exact cause of vasculitis isn’t fully understood. But what medical professionals do know is there are two main categories of vasculitis: primary vasculitis and secondary vasculitis. Medical News Today says that primary vasculitis means there is no known cause.
Secondary vasculitis, on the other hand, means it developed because of another disease such as an infection (such as hepatitis C), an allergic reaction to some medication, an immune system disorder (such as lupus or rheumatoid arthritis), or some cancers (such as lymphoma or leukemia). The source also says the following are specific types of vasculitis:
- Behcet’s disease
- Buerger’s disease
- Central nervous system (CNS) vasculitis
- Churg-Strauss syndrome
- Cryoglobulinemia
- Giant cell arteritis
- Henoch-Schönlein purpura
- Kawasaki disease
- Takayasu’s arteritis
- Wegener’s granulomatosis
- Rapidly progressive glomerulonephritis
Other Signs and Symptoms to Know
Each type of vasculitis can affect the body differently. For example, the Mayo Clinic says if your digestive system is affected, you may experience pain after eating or develop blood in the stool.
When the ears are affected you may develop a ringing in the ears, dizziness, or even abrupt hearing loss. Vasculitis can also affect the eyes causing them to look red, become itchy, or burn. The source also notes, “Giant cell arteritis can cause double vision and temporary or permanent blindness in one or both eyes.”
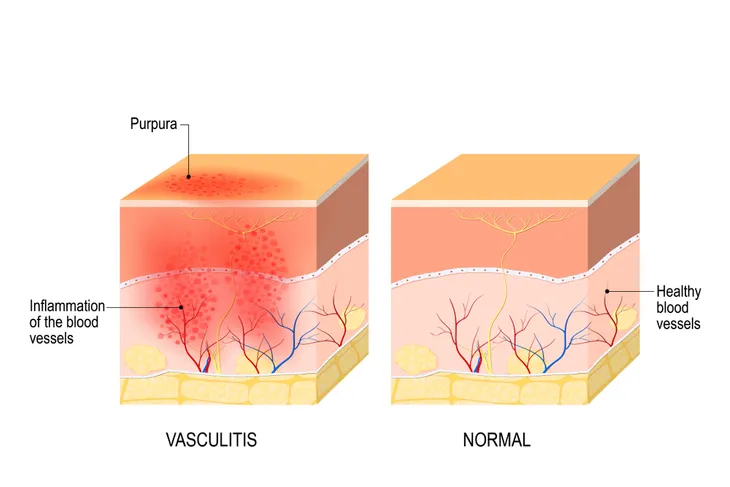
Vasculitis can also affect the hands or feet, causing numbness or weakness and it can affect the lungs, resulting in shortness of breath or coughing up blood. Finally, the condition can also affect the skin, causing bleeding under the skin which appears as red spots on the surface.
When to See a Doctor
Developing any new abnormal symptoms can be alarming. While you may be tempted to self-diagnose, it’s always best to get checked out by a medical professional. If you develop any of the above signs or symptoms, or any symptoms that concern you, contact your doctor right away.
The Mayo Clinic notes that some types of vasculitis can worsen quickly which makes an early diagnosis even more important. Early intervention is also important for starting an effective treatment plan as soon as possible.
Possible Risk Factors
Although vasculitis can happen to anyone, certain factors may increase your risk. For starters, age can play a role. For example, the Mayo Clinic explains that giant cell arteritis rarely develops before 50-years old whereas Kawasaki disease is more common in children under 5-years old.
Having a family history of certain types of vasculitis can also increase your risk. As can having an immune disorder. Smoking, taking certain medications, and having hepatitis B or C can also increase your risk. If you’re worried about your risk for vasculitis, talk to your doctor.
Possible Complications
As we mentioned, early intervention is key. Some types of vasculitis can cause serious complications, especially if left untreated. For starters, some types of vasculitis can cause damage to major organs which can be life-threatening.
Vasculitis can also cause blood clots, and more rarely, aneurysms. Further, untreated giant cell arteritis may lead to vision loss or complete blindness. All the more reason to see your doctor for a proper diagnosis and treatment plan.
How Is Vasculitis Diagnosed?
If your doctor suspects you may have vasculitis there are a variety of tests they can do to help confirm a diagnosis. A doctor typically starts by reviewing your medical history, and current symptoms, as well as a physical exam.
They’ll also likely request specialized laboratory tests to test your blood for abnormalities, which can develop when vasculitis is present, explains the Cleveland Clinic. Your doctor will be looking for anemia (low red blood cell count), a high white blood cell count, a high platelet count, as well as signs of liver or kidney trouble. The source also notes that your doctor may require additional testing to confirm a diagnosis such as biopsies, X-rays, and blood vessel and heart scans.
How Is Vasculitis Treated?
If vasculitis is confirmed, your medical team will create a treatment plan tailored to your type of vasculitis. Treatment will vary depending on the type of vasculitis as well as the area and organs that are affected.
The Mayo Clinic explains that the goal of treatment is to control the inflammation and manage “any underlying conditions that may be triggering the vasculitis.” Since some types of vasculitis can worsen quickly, it’s vital that you follow your treatment plan closely. Early intervention is key!
Treatment Options for Vasculitis
As mentioned, treatment will vary depending on your type but most involve some type of medication that can help control the inflammation. Ultimately, your doctor will determine which medication is best for you. It’s also worth noting that medications that treat vasculitis often have strong side effects so be sure to discuss this with your doctor so you know what to expect.
The Mayo Clinic also notes that surgery may be necessary if your vasculitis causes an aneurysm. The surgery can help reduce the risk of it rupturing. Surgery may also be necessary if your vasculitis causes blocked arteries. The goal is to restore blood flow to the affected area.
Coping With Vasculitis
Receiving any medical diagnosis can be worrisome, especially when you’re experiencing severe symptoms. This is why leaning on a support system is so important. Discussing your condition with family and friends may help you cope but you can also connect with other people who are living the same condition. Ask your medical team to connect you with a support group.
The Mayo Clinic also notes that the side effects of your medication may be challenging to live with so it’s important to learn how to cope with that too. Some ways you can do this include eating a healthy diet, exercising regularly, and getting routine vaccinations. The source explains, “Keeping up to date on vaccinations, such as for the flu and pneumonia, can help prevent problems that can result from your medications, such as infection.”
Can Vasculitis Be Prevented?
According to the National Heart, Lung, and Blood Institute (NHLBI), some types of vasculitis cannot be prevented because they’re caused by autoimmune disorders. That said, “depending on what caused the vasculitis, some types can be prevented from flaring up,” explains the source.
The source notes that healthy lifestyle changes may be recommended, such as quitting smoking. While this is no easy feat, there are resources available to help you. Adopting a heart-healthy lifestyle may help too. This should include:
- Eating heart-healthy foods
- Managing your blood pressure and cholesterol
- Maintaining a healthy weight
- Exercising regularly
- Managing stress
- Getting enough good quality sleep