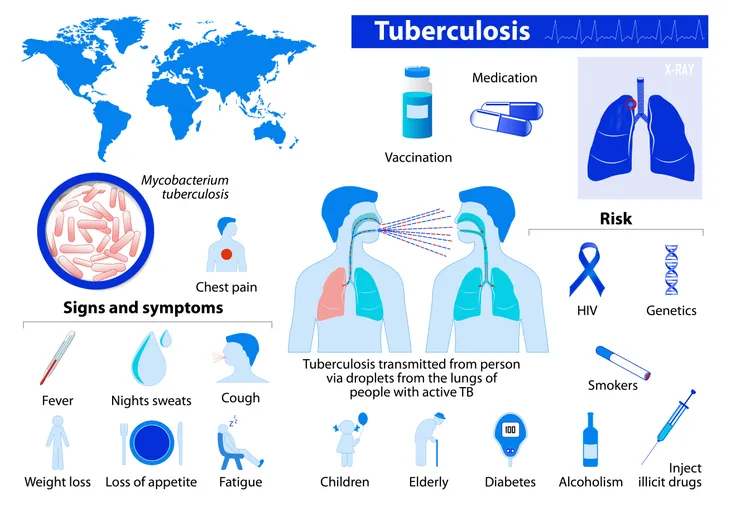
Tuberculosis, which is commonly referred to as TB, is an infectious disease that primarily affects the lungs, although it can spread to other areas of the body such as the kidneys, brain, and spine.
Tuberculosis is considered an airborne pathogen, as the bacteria that cause the disease can spread from person to person through the air, infecting an estimated 9 million people worldwide each year. Although certain individuals are more at risk of developing tuberculosis than others (as we’ll discuss later), anyone can get it. So it’s important to recognize the symptoms in order to seek appropriate medical treatment.
Symptoms
A Cough that Lasts 3 or More Weeks
There are two types of tuberculosis: latent tuberculosis and active tuberculosis. With latent tuberculosis, people become infected but do not actually develop the disease, and therefore have no symptoms. Those with active tuberculosis, however, do become sick after being infected with the disease.
One of the primary symptoms of active tuberculosis is a bad cough that persists for a period longer than 3-weeks. With this cough, the Government of Canada indicates it may cause you to sometimes cough up blood or phlegm, “thick liquid that comes up from your lungs or airways.”
Chest Pain When Coughing or Breathing In
As stated in the introduction, tuberculosis most commonly affects the lungs, causing respiratory-related symptoms such as coughing (which we just talked about) and chest pain.
This chest pain may be felt when you are coughing, but can also occur when you breathe in, which Breathing Matters says is “caused by inflammation of the membranes lining your lungs,” known as pleurisy. HealthCommunities.com indicates pleurisy “usually develops soon after initial infection” and may also be accompanied by shortness of breath (dyspnea).
Unintentional Weight Loss
With active tuberculosis, it is not uncommon for there to be “a sudden dip in the appetite of an individual,” says OnlyMyHealth.com. In addition to loss of appetite, they may also experience nausea and vomiting.
As a result of these symptoms, people with tuberculosis tend to lose weight rapidly and unintentionally. Should this dramatic drop in weight occur before diagnosis and treatment of the disease, the source indicates that “the likelihood of relapse becomes significantly high,” even after they begin drug therapy.
Fatigue
Fatigue is another common symptom of active tuberculosis. This may present itself a variety of forms, including loss of energy, feeling tired all the time, and weakness.
As there are many different factors and conditions that can cause fatigue, it may be hard to identify as being caused by tuberculosis. But, if you notice yourself experiencing feelings of tiredness and weakness in combination with other symptoms on this list, be sure to make an appointment with your physician.
Fever
As the body attempts to fight off a tuberculosis infection, a high fever commonly develops, with a temperature of 100.4-degrees Fahrenheit or higher (38-degrees Celsius). This fever may be accompanied by symptoms like chills and night sweats. With night sweats, Express says that people “typically wake in the night to find their bed clothes drenched.”
One possible cause of night sweats in people with tuberculosis is a lack of air circulation around the body while sleeping, where excess body heat from a fever can’t escape, resulting in sweating. Night sweats may also be due to the production of cytokines, “proteins that are released to help regulate the body’s immune response to the infection,” says AZCentral.com.
Symptoms of Active Tuberculosis Outside of the Lungs
Although tuberculosis most commonly affects the lungs, it’s possible for it to occur in other organs of the body, including the kidneys, brain, spine, or lymph nodes. When this happens, the symptoms are dependent on what area is affected.
With tuberculosis of the spine, for instance, the Mayo Clinic says it “may give you back pain,” whereas tuberculosis in the kidneys “might cause blood in your urine.” Or, if tuberculosis is affecting the lymph nodes, WebMD indicates, “…your neck may get swollen.”
Risk Factors
Close Contact with Someone Who Has Tuberculosis
As mentioned earlier, tuberculosis is an airborne pathogen, meaning it can be passed from person to person through the air. As such, one of the primary risk factors of getting the disease is being around those who have active tuberculosis.
This includes people you live with, such as family or roommates, as well as others you encounter on a regular basis, such as friends and co-workers, because tuberculosis “…is spread most easily in closed spaces over a long period of time,” says the American Lung Association.
Weakened Immune System
According to the Mayo Clinic, “A healthy immune system often successfully fights TB bacteria, but your body can’t mount an effective defense if your resistance is low.” Unfortunately, your immune system can be compromised by a variety of different conditions and factors, leaving you more susceptible.
These include HIV or AIDS, diabetes, severe kidney disease, head and neck cancers, cancer treatment (i.e., chemotherapy), medications for organ transplant, malnutrition, and certain drugs that are used to treat conditions, such as rheumatoid arthritis, Crohn’s disease, and psoriasis. WebMD adds, “Babies and young children also are at greater risk, because their immune systems aren’t fully formed.”
Living in or Traveling to Certain Areas
People are also at an increased risk of developing tuberculosis if they live in or travel to certain countries “that have high rates of tuberculosis and drug-resistant tuberculosis,” says the Mayo Clinic.
According to MedicalNewsToday.com, the areas of the world where tuberculosis is most prevalent include: Africa (West Africa and sub-Saharan Africa, in particular), Afghanistan, Southeast Asia (including Pakistan, India, Bangladesh, and Indonesia), China, Russia, South America, and the Western Pacific region (including the Philippines, Cambodia, and Vietnam).
Lack of Medical Care
People who have poor access to health care are also more likely to contract tuberculosis, such as those who “receive a low or fixed income, live in a remote area,…or are homeless,” says the Mayo Clinic. Individuals who have recently immigrated to the United States are also at a higher risk, particularly if they are coming from any of the countries previously mentioned that have high rates of tuberculosis.
Not only are these groups of people more likely to develop tuberculosis, but because of their lack of access to proper medical care, they are also less likely to receive the diagnosis and treatment they need.
Substance Abuse
People who abuse alcohol and intravenous (IV) drugs are also at a higher risk of contracting tuberculosis, as these substances weaken the body’s immune system, making them more vulnerable to infection.
MedicalNewsToday.com indicates, “Tobacco use has also been found to increase the risk of developing active TB.” In fact, the source says, “About 8 percent of TB cases worldwide are related to smoking.” The Mayo Clinic adds that tobacco use greatly increases a person’s risk of dying from the condition as well.
Where You Work or Live
Where you live or work can also be a factor that increases your risk of getting tuberculosis. According to the American Lung Association, this means people who “reside in facilities or institutions that house people who are at high risk for TB.”
Such locations include hospitals, where health care workers regularly come into contact with people who are ill. Other places include those that are overcrowded and have poor ventilation, such as homeless shelters, prisons, nursing homes, and immigration centers. The Mayo Clinic adds that those living in refugee camps are at an especially high risk as they are “weakened by poor nutrition and ill health and living in crowded, unsanitary conditions.”