Ulcerative colitis is an inflammatory bowel disease that, similar to Crohn’s disease, can cause irritation, inflammation, and ulcers in the large intestine. This chronic disease is a result of the immune system’s overactive response, and is unfortunately incurable. People with this condition will struggle with symptoms throughout their entire life. Thankfully, it can be managed with treatment, but the first step is to recognize the symptoms.
Ulcerative colitis isn’t typically a fatal disease and the symptoms can vary from person to person with about half of all ulcerative colitis patients experiencing mild symptoms. However the following symptoms can have a major impact on your general health and quality of life…
1. Abdominal Pain
Like Crohn’s disease, during flare-ups, ulcerative colitis causes ever-present stomach cramping and stabbing pain, which is similar to the feeling of having to take an explosive bowel movement without being able to. During times of remission, abdominal discomfort will virtually disappear.
2. Constipation
Another uncomfortable symptom associated with ulcerative colitis is constipation. This is when a person make infrequent or uncomfortable bowel movements. John Hopkins Medicine says a person is considered constipated if they have bowel movements fewer than three times a week. The stool is also typically dry and hard, which is not normal for people with healthy bowel movements.
3. Severe Dehydration
Unfortunately, ulcerative colitis can also put you at higher risk of severe dehydration. Some factors that can lead to dehydration include frequent or watery diarrhea, not drinking enough water, or excessive sweating. If your body is unable to maintain a proper amount of hydration after things like bowel movements, sweating, and even moisture in breath, then dehydration can occur.
4. Rectal Pain and Bleeding
Ulcerative colitis that causes pain and inflammation only in the area of the anus (or rectum) is known as proctitis. This form of the condition is known to cause rectal bleeding as well as the constant feeling of having to take an urgent bowel movement.
5. Sudden and Significant Weight Loss
Pancolitis is a form of colitis that results in bouts of diarrhea so explosive, and sometimes bloody, that the patient will suffer from severe and sudden weight loss as well as associated fatigue due to dehydration and decreased absorption of calorie from foods.
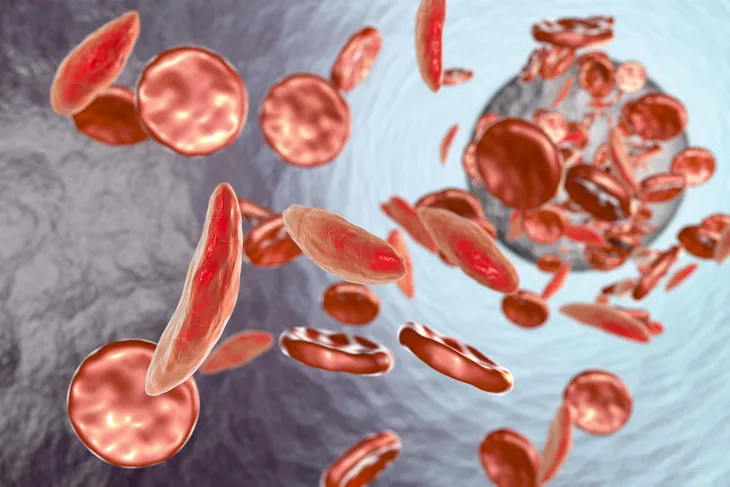
6. Anemia
Anemia, usually of severe iron deficiency type, can occur if an ulcerative colitis patient suffers from bloody and explosive diarrhea. Due to the constant blood loss and bleeding from the rectum, the sufferer can become very weak. If you suspect you might be anemic, your doctor should perform a blood test to verify this possibility.
7. Urgent Diarrhea
Unfortunately, for many ulcerative colitis sufferers, the urgency to defecate is so overwhelming and pressing that they are unable to be too far from a bathroom, for even short periods of time. During periods of flare-ups, many patients are too embarrassed to leave the house, fearing an accident.
8. Fatigue
It’s common, due to explosive diarrhea as well as anemia, for those with ulcerative colitis to suffer from severe fatigue. They may also suffer from malnutrition, because they are unable to absorb the nutrients from the food they consume.
9. Fever
Oftentimes, when colitis flare-ups cause inflammation of the colon and the rectum, a mild to high temperature can develop as the body tries to fight the malnourishment, fatigue, nausea, and general malaise associated with the condition.
10. Inflammation of Major Organs
Other major symptom of ulcerative colitis are gassiness, bloating, and inflammation that starts in the colon. However, inflammation can extend to other organs, such as the upper digestive tract, cause pain and blockages in the small intestine.