Abdominal pain is a common reason to visit the doctor, whether in an office or emergency department visit. According to the National Ambulatory Medical Care Survey, abdominal pain was the reason for 1.5-percent of all visits to doctor’s offices. Research at the University of Connecticut Medical School revealed abdominal pain accounted for 5-percent of all visits to the emergency department. Of those visits to the emergency department, approximately 10-percent required surgery.
The top 10 causes of lower right abdominal pain are…
1. Appendicitis
Appendicitis is inflammation of the appendix. The appendix is a worm-like pouch that projects from the ascending colon, which is the first section of the colon (large intestine). No one knows the specific purpose of the appendix. Associated symptoms may include fever, nausea, vomiting, and loss of appetite (anorexia). Surgery to remove the appendix (appendectomy) is the usual outcome of an episode of appendicitis.
If surgery is delayed, the appendix could rupture and spread an infection throughout the abdomen (peritonitis). Recent research in Finland, published in the Journal of the American Medical Association, found antibiotic treatment of appendicitis to be as effective as surgery to remove the appendix.
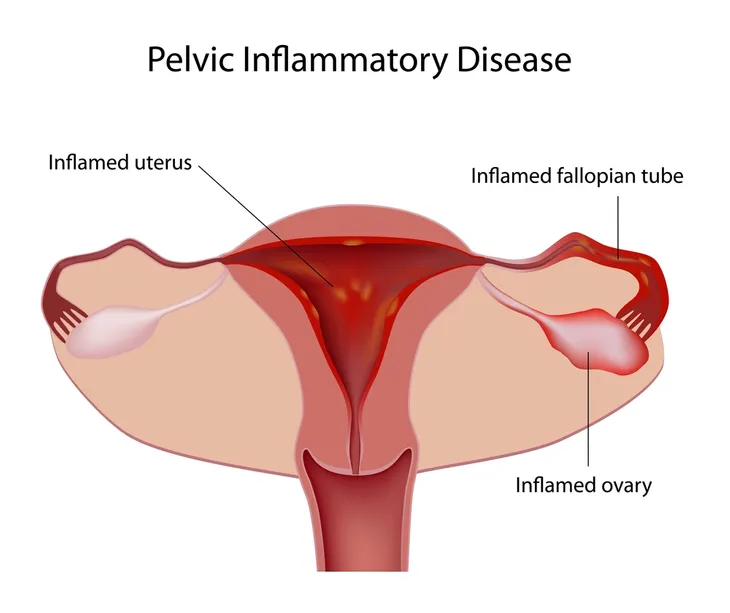
2. Pelvic Inflammatory Disease (PID)
Pelvic inflammatory disease (PID) is caused by an infection of the upper portion of the female reproductive tract. The U. S. Centers for Disease Control and Prevention (CDC) estimates it affects 1.5-million women annually. The most common causes of PID are the sexually transmitted infections (STIs) chlamydia and gonorrhea. Associated symptoms of PID may include vaginal discharge or bleeding, fever, vomiting, back pain, and painful intercourse (dyspareunia).
In some women, symptoms are mild or even absent. Women with PID may be treated with oral or intravenous antibiotics, depending on the severity of symptoms. Complications of PID include chronic pelvic pain, infertility, and ectopic pregnancy. An ectopic pregnancy occurs outside of the uterus and is a surgical/medical emergency.
3. Colon Cancer
Colon cancer is cancer of the large intestine (colon). Most cases of colon cancer develop from polyps, which are growths in the lining of the colon that protrude into the lumen (opening) of the colon. There are several types of colon polyps, with adenomatous polyps being the most common. Adenomatous polyps are considered precancerous and have the potential to develop into colon cancer. Symptoms suggestive of colon cancer—include changes in bowel habits (diarrhea or constipation) or stool caliber (can be pencil-thin), rectal bleeding or blood in the stool, fatigue, and unexplained weight loss.
Screening for colon cancer should commence at age 50 and may be done with the following methods—fecal occult blood test, barium enema, flexible sigmoidoscopy, colonoscopy, or virtual colonoscopy. The best of these screening methods is colonoscopy, because the entire colon is visualized and polyps can be removed simultaneously. Colonoscopy can be diagnostic, as well as curative.
4. Kidney Stones
Kidney stones, also referred to as nephrolithiasis, are small, hard mineral deposits that form inside the kidneys. They form when there is a decrease in urine volume and/or an excess of stone forming substances in the urine. The types of kidney stones include calcium oxalate, calcium phosphate, uric acid, struvite, and cystine. Associated symptoms may include hematuria (blood in the urine), dysuria (painful urination), nausea, vomiting, urinary frequency, and urinating small amounts.
Kidney stones are usually diagnosed with a computed tomography (CT) scan of the abdomen. Most kidney stones are small enough to pass in the urine. Treatment usually consists of increasing water intake and pain medications. Some individuals are asked to strain their urine to recover stones for analysis. Kidney stones too large to pass in the urine can be treated with lithotripsy or surgical removal.
5. Inguinal Hernia
An inguinal, or groin, hernia is a condition in which part of the intestines protrudes through a weak point in the abdominal muscles. They are the most common type of hernia and can be unilateral or bilateral. Males are much more likely to develop inguinal hernias than females. Signs and symptoms of an inguinal hernia may include a mass or bulge in the groin, aching sensation over the bulge, and occasionally pain or swelling in the testicles. The bulge in the groin becomes more obvious when standing, especially with coughing or straining.
A physical exam is all that is needed to diagnose an inguinal hernia. Surgery, open or laparoscopic, is usually indicated for repair of an inguinal hernia. Today, the majority of hernia repairs are of the laparoscopic type. Inguinal hernias are repaired to prevent complications such as incarceration or strangulation.
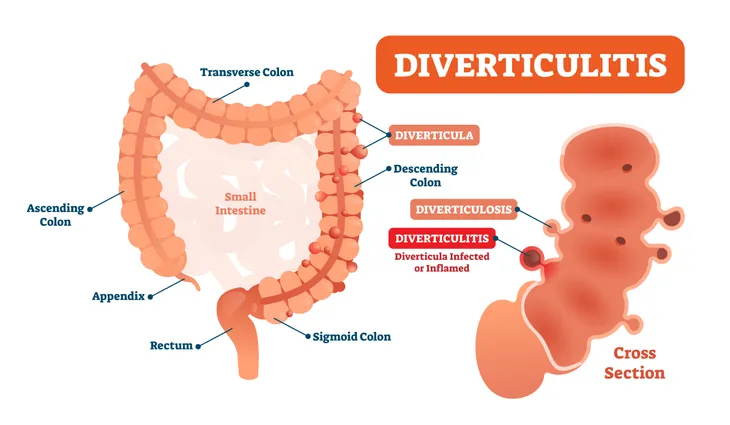
6. Diverticulitis
Diverticulitis is inflammation or infection in one or more small pouches in the colon (large intestine). As we age, the muscular walls of the colon weaken leading to the formation of small pouches in the colon referred to as diverticulosis. Associated symptoms of diverticulitis include abdominal pain, fever, nausea, vomiting, loss of appetite (anorexia), and marked changes in bowel habits (mostly constipation, but can also be diarrhea).
Mild cases may be treated as an outpatient with a clear liquid diet and 7- to 10-days of oral antibiotics. Hospitalization is required for moderate to severe cases and consists of bowel rest, pain management, and intravenous antibiotics. Complications of diverticulitis include abscess formation and bleeding. These complications, and frequently recurring episodes, of diverticulitis may require surgery to remove the diseased parts of the colon.
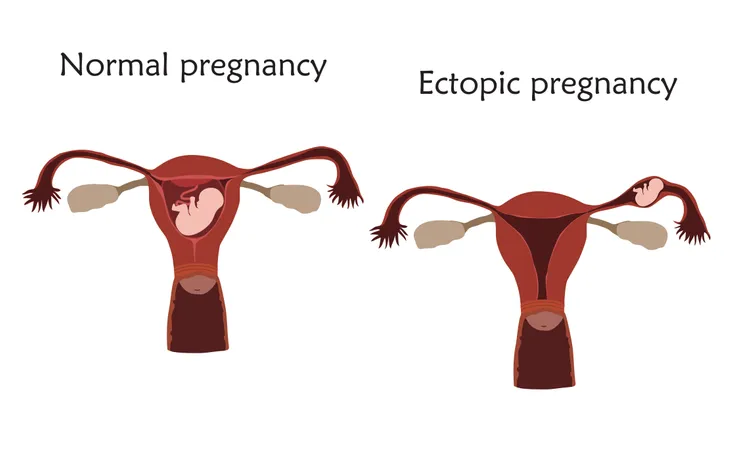
7. Ectopic Pregnancy
An ectopic, or tubal, pregnancy occurs when a fertilized egg implants in tissue outside the womb, or uterus. It most often occurs in one of the two fallopian tubes. Other sites the condition can occur include the abdominal cavity, ovary, or cervix.
Ectopic pregnancy occurs when pregnancy cannot continue to birth (term) because the growing tissue may lead to the rupture of the fallopian tube, which could cause life-threatening blood loss. An associated symptom is vaginal bleeding. A pelvic ultrasound can confirm the diagnosis. Emergency surgery is needed to remove the ectopic tissue and prevent life-threatening complications.
8. Inflammatory Bowel Disease
Inflammatory bowel disease involves chronic inflammation of part or all of the digestive tract. There are two types of inflammatory bowel disease: ulcerative colitis and Crohn’s Disease. Symptoms associated with inflammatory bowel disease include diarrhea, fatigue, fever, blood in the stool, decreased appetite, and unintended weight loss. The exact cause of inflammatory bowel disease is unknown. The disease is easily diagnosed by biopsy during colonoscopy.
There is no cure for inflammatory bowel disease. The goal of treatment is the reduction of inflammation. Sulfasalazine and corticosteroids are the mainstays of treatment for inflammatory bowel disease. Partial colectomy (removal of the colon) is sometimes necessary for the treatment of severe disease. Complications of inflammatory bowel disease may include bowel obstruction, ulcers, and fistulas (an abnormal connection between body parts).
9. Endometriosis
Endometriosis is a disorder in which tissue that normally lines the uterus grows outside the uterus. It can be found on the ovaries, fallopian tubes, or the intestines. The cause of endometriosis is unknown. Associated symptoms include heavy periods (menorrhagia) and infertility. Endometriosis can be diagnosed through laparoscopy, which is visual examination of the abdomen. Laparoscopy is a surgical procedure characterized by a physician inserting a thin, lighted tube through a small incision in the abdomen.
There is no cure for endometriosis, but treatment can improve the symptoms. Effective treatments include pain medications and hormone therapy. Surgery to remove the uterus (hysterectomy) and ovaries (oophorectomy) is an option in severe disease. The main complication of this disorder is impaired fertility.
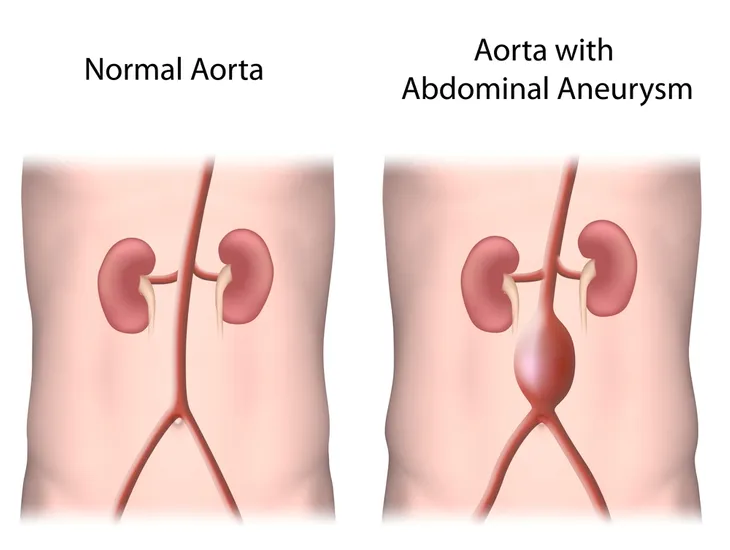
10. Abdominal Aortic Aneurysm
An abdominal aortic aneurysm (AAA) refers to an enlarged area in the lower portion of the aorta, the largest artery in the body. The enlarged area is caused by weakness in the muscular walls of the aorta. The exact cause of this condition is unknown. Risk factors for the development of this aneurysm include smoking, high blood pressure (hypertension), and male gender. Most individuals with an abdominal aortic aneurysm have no symptoms until it ruptures. Symptoms of rupture may include dizziness, nausea, vomiting, syncope (fainting), rapid heart rate (tachycardia), and shock.
Unfortunately, the mortality, or death, rate for a ruptured AAA is around 90-percent. Occasionally, an abdominal aortic aneurysm is an incidental finding on an imaging study obtained for another reason. If this is the case, the aneurysm size can be followed periodically. Abdominal aortic aneurysms less than 5.5-centimeters should be considered for repair.