News stories of the superbug MRSA, or Methicillin-Resistant Staphylococcus Aureus, are almost as rampant as the strain of drug-resistant staph bacterial infection itself. With new stories emerging almost daily concerning the MRSA cropping up in elementary schools and athletic locker rooms, it’s not wonder this new “super bug” is on everyone’s mind.
Let’s examine the causes, symptoms, treatment, risk factors, and prevention for MRSA…
1. What is MRSA?
Methicillin-Resistant Staphylococcus Aureus (or MRSA) is strain of staphylococcus aureus (or staph) bacterium that infects various parts of the body with sores, boils, or mild skin infections. Typically, we all carry staph bacteria on our bodies (and inside our noses) without threat of infection.
However, staph bacterium is dangerous if it enters the body via wound or cut and causes an infection. A primary cause of skin infections among Americans, staph infections are usually minor. But severe forms of staph infection, like MRSA, result with the infection of surgical wounds, organs (i.e., lungs causing pneumonia), and bloodstream of those with weakened immunity.
2. What Makes MRSA Resistant?
What differentiates MRSA from other bacterium is the fact that it’s hard to treat and often resistant to antibiotics. Initially identified in 1961, MRSA was once treated with antibiotics, but over time the strain became resistant and adapted to the penicillin, oxacillin, methicillin, amoxicillin, and other common antibiotics used for its destruction.
This means that MRSA has the potential to spread quickly via compact communities—such as hospitals, community centers, residential homes, schools, and anywhere where close quarters are shared and inhabitants come into frequent skin-to-skin contact.
3. How is MRSA Contracted?
MRSA spreads via skin-to-skin contact. That means you can get it, for example, by touching an individual with MRSA bacterium on their skin. The Centers for Disease Control and Prevention estimates that 2-percent (or roughly every 2 in 100) carries MRSA bacteria on their skin and inside their noses. However, most will never become infected.
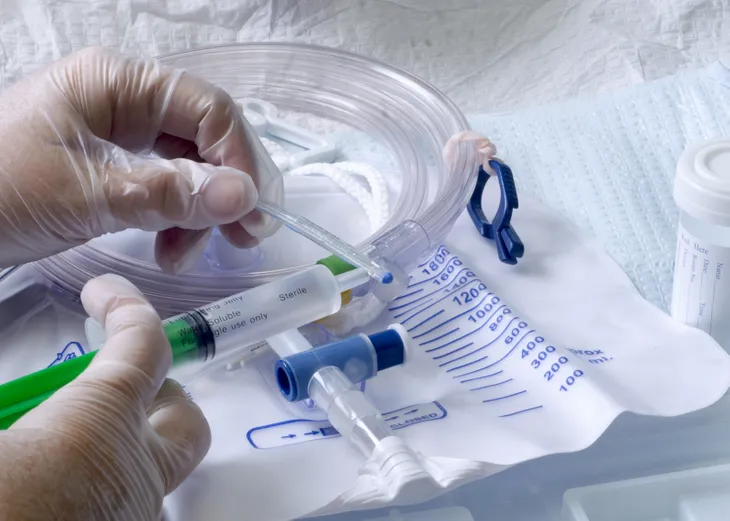
You can also contract MRSA by coming into contact with objects containing the bacterial strain. For instance, in hospitals and nursing homes, feeding tubes and catheters are prime culprits of staph bacterium, which is why medical professionals have been taking extra precautions to prevent the spread of MRSA to vulnerable patients.
4. The Risk of Hospital MRSA
MRSA that occurs in a hospital or nursing home setting is referred to as HA-MRSA. It typically strikes the most vulnerable individuals—patients who’ve received an invasive medical tool or device such as a feeding tube, artificial joint, intravenous fluids, or urinary catheters.
Elderly patients and ill individuals with compromised immune systems are also at heightened risk of MRSA entering the body if they suffer a wound or use a feeding tube. This is why homecare facilities and long-term residential care patients within are also at increased risk of contracting HA-MRSA.
5. The Risk of Community-MRSA
MRSA that’s contracted in non-medical environments is referred to as C-MRSA (or Community-MRSA). The risk factors for C-MRSA are highest for those living and recreating in crowded, unsanitary environments.
This includes gyms, community centers, athletic locker rooms, and physical training facilities (i.e., military or wrestling). This from of bacterial infection is typically contracted via an open wound, scrape, or abrasion due to skin-to-skin contact with an individual carrying MRSA on their body.
6. Primary Symptoms of MRSA
As mentioned, MRSA occurs at a sight of infection. This means the symptoms will differ depending on the area of infection. Many MRSA infections get into minor cuts or scrapes, insect bite, or even pimples. These will start as topical skin infections with the formation of a skin rash, or tiny red bumps that appear similar to pimples or spider bites.
However, if the rash turns into boils, or forms a deep abscess inside the body, a life-threatening infection can result in the bloodstream, joints, bones, surgical wounds, lungs, and heart valves. See your doctor immediately at the first sign of infection.
7. Treatment of MRSA
Even though MRSA is often drug-resistant, medical science continually works to find new ways to fight the infection. In order for proper diagnosis, your doctor will likely take a tissue sample or liquid from the infected area to test for presence of MRSA bacteria.
If either HA-MRSA or C-MRSA is identified, your doctor may still prescribe an antibiotic to see if the infection will respond. If an abscess occurs superficially, your doctor may perform drainage. In cases of an interior abscess, surgery and patient isolation in a sterile environment may be required.
 Shutterstock/Soru Epotok
Shutterstock/Soru Epotok8. Preventing the Spread of MRSA
If you find yourself regularly in close quarters (i.e., a hospital, gym, or residential facility) hygiene is essential to avoid the contraction of MRSA. Wash your hands frequently and thoroughly with soap and water, or use a hand sanitizer with 62-percent alcohol (minimum).
If you suffer a superficial cut or abrasion, clean immediately and cover with a clean, dry bandage to keep out bacteria. In athletic facilities, avoid sharing towels, clothing, and personal hygiene products (i.e., razors). Take a shower immediately after workouts and practices, and change into clean, dry clothes to avoid the spread of bacteria.