Temporomandibular joint disorder (TMJ) is a mouthful, and ironically it’s located right near the mouth! This particular joint is on the jawbone which connects to the skull. Every person has one on each side of their jaw. For people who suffer from temporomandibular joint disorder, it causes pain on both sides of their mouth and is usually due to genetics, arthritis, or some sort of jaw injury, says Mayo Clinic.
TMJ disorders aren’t something we hear about all that often, but it’s actually quite common, especially for people who tend to clench or grind their teeth. Here’s a look at everything you need to know about temporomandibular joint disorder….
1. What is it?
As we previously mentioned, the temporomandibular joint is located on the side of the jaw. We each have one on each side of the jaw. Mayo Clinic describes it as a “sliding hinge, connecting your jawbone to your skull.” According to the Canadian Dental Association, the TMJ is considered one of the most complex joints in the body. It not only moves forward and backwards, but it can also rotate and move side to side. With a little help from some other muscles and ligaments, it also allows us to chew, speak, yawn, and swallow. A temporomandibular joint disorder is when someone suffers from pain in their jaw joint and the muscles that help open and close the jaw, or any other jaw movements.
To locate your temporomandibular joint, place two fingers on your cheek, right in front of your ears, and then open and close your mouth. You should be able to feel a rounded joint that moves as the mouth opens and closes. “What you’re feeling are the rounded ends of the lower jaw as they glide along the joint socket of the temporal bone, which is the part of the skull that contains the inner ear and the temple,” writes Kid’s Health.
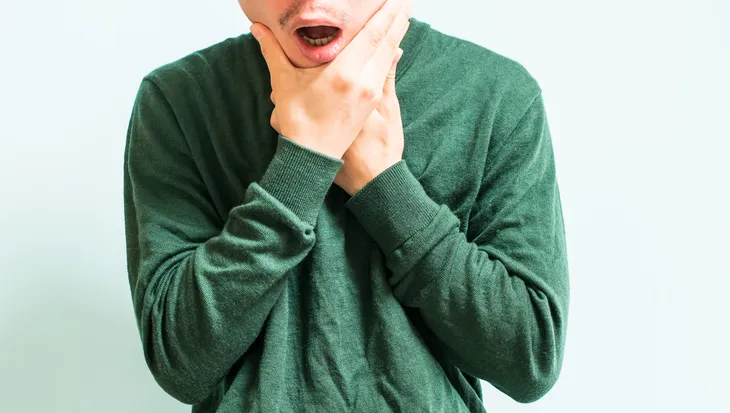
2. Most Common Symptoms
The most common symptom of temporomandibular joint disorder is pain in the head, neck, and of course, jaw. A person who suffers from this disorder will experience pain and tenderness on their joint and jaw, as well as around their ears. WebMD points out that this pain can be temporary or last years, it all depends on the person and the extent of their disorder. It can also affect just one side or both sides. It could make it hard to chew food, or in some cases, cause lock jaw which makes it difficult to even open or close the jaw. Other symptoms include swelling in the face, a “tired feeling” in the face, or a sudden dislocation in the bite where the upper and lower teeth no longer line up and fit together properly making it uncomfortable to close the mouth. “You may also have toothaches, headaches, neck aches, dizziness, earaches, hearing problems, upper shoulder pain, and ringing in the ears (tinnitus),” writes WebMD.
The Mayo Clinic also points out that TMJ disorders can also cause “a clicking sound or grating sensation” when a person opens and closes their jaw. If you’re one of those people who has a clicking sound when they chew, don’t fret, lots of people have that who don’t have a TMJ disorder.
3. Causes
For the most part, it’s unclear what exactly causes temporomandibular joint disorders. While it can be brought on by grinding the teeth or clenching the jaw repeatedly, it’s often credited to being caused by some kind of injury to the jaw, joint, or muscles in the head and neck. For example, a person who has suffered a massive blow to the head or whiplash might develop a TMJ disorder as a result. WebMD also lists “movement of the soft cushion or disc between the ball and socket of the joint, arthritis in the joint,” and stress which causes someone to tighten their facial and jaw muscles, as well as clench their teeth.
Medical News Today points out that there is a argument to be made for lifestyle causes, like people who play instruments. According to the source, violinists have been known to be at a higher risk for developing a TMJ disorder than the average person because they hold their instrument under the jaw and can be quite tense or rigid while they play which causes repeated stress and strain.
4. Prevention
Many people, even kids will develop temporomandibular joint disorder when they repeatedly and unconsciously grind their teeth or clench their jaw. It’s important to note that this doesn’t happen to every person who does this! But for those that do, there are a few ways that it can be prevented.
Kid’s Health explains that kids might start to notice there are particular times when they engage in these behaviors. For example they might do it when they are stressed while writing a test or when they’re angry. If they are able to recognize when it happens they can can be more conscious about stopping them. If these examples are the case, then teach a child or an adult for that matter, better ways to handle their stress. They could start getting more exercise or new breathing mechanisms. You could also consult with your dentist for more ideas.
5. How to Manage the Pain
Not surprisingly, the pain associated with TMJ disorder can be quite uncomfortable and just a plain old nuisance. The Canadian Chiropractic Association offers up some advice on how someone could treat or even reverse some of the pain. For starters, since it affects the jaw and can be irritated when opening and closing the jaw, limit this behavior by eating softer foods. A patient could also try “applying ice packs, avoiding extreme jaw movements, learning techniques to relax and reduce stress, and practicing gentle stretching of the jaw to help increase movement,” writes the source. You should also refrain from chewing gum, biting fingernails or chewing your cheeks.
The Canadian Chiropractic Association also suggests intraoral myofascial release which is a technique used by some healthcare professionals like chiropractors to release muscles around the joint. There’s also spinal manipulative therapy, soft tissue massage, and a few exercises (which we will get to next) that can help relieve some of the pain.
6. Exercises to Help Manage Pain
The pain associated with TMJ disorders can be quite uncomfortable and awkward because it’s surrounded by muscles we need to use all the time. While a mouth guard is a common for of treatment for people with TMJ, Helathline cites a 2010 study published in the Journal of Dental Research which found that exercises could help increase the range of motion in people with disc displacement more than a mouth guard.
The American Academy of Family Physicians (AAFP) and Royal Surrey County Hospital provide some easy exercises that could help relieve any pain associated with a TMJ disorder and increase movement in the jaw. The exercises they have listed are called “resisted mouth opening, resisted mouth closing, tongue up, side-to-side jaw,” and “forward jaw movement.” To find out more about how to perform these exercises, click here. The source notes that none of these exercises should be painful and that if any of them do cause pain, you should consult with your doctor before continuing to do them.
7. When to See a Doctor
A temporomandibular joint disorder can be easily managed and doesn’t really require much in terms of healthcare assistance. But the Mayo Clinic does advise anyone with persistent pain and tenderness or someone who has trouble opening and closing their jaw, to go seek medical attention either from a doctor, dentist or TMJ specialist. These healthcare professionals will help figure out what is causing the problem and if there are any possible treatments.
8. Common Risk Factors
We already discussed some of the possible causes for TMJ disorder, but are their any risk factors? For starters, for whatever reason, it affects more women than men and it’s more common among people between the ages of 20 and 40. But the Mayo Clinic lists a few other risk factors like various types of arthritis, like rheumatoid arthritis and osteoarthritis. Anyone who is already suffering from these forms of arthritis could be more likely to develop a temporomandibular joint disorder.
Also, anyone who has suffered a jaw injury or is known for being a chronic teeth grinder or someone who frequently clenches their jaw. Lastly, “certain connective tissue diseases that cause problems which may affect the temporomandibular joint,” writes the Mayo Clinic.
9. Home Treatments
These at home treatments are similar to what we discussed as part of pain management earlier on in the article. There isn’t really a cure for TMJ disorder but rather things that can be done to help alleviate the pain. A lot of these pain relieving techniques can be done at home which makes it a fairly manageable condition. Many people resort to over-the-counter medication like non-steroidal anti-inflammatory drugs to relieve the muscle pain and swelling. You could also try applying a hot or cold compress to the side of the face for about 10-minutes. If your dentist has given you jaw stretches to do, try doing these after applying a compress. Follow it up with a warm towel or washcloth to the side of the face, and repeat the process a few times throughout the day.
When it comes to diet, an easy thing to do is to swap chewy or crunchy food for something a little softer. WebMD lists things like “yogurt, mashed potatoes, cottage cheese, soup, scrambled eggs, fish, cooked fruits and vegetables, beans, or grains,” as good go-to food items. You could also cut the food into smaller pieces so it requires less chewing. The same source lists not resting the chin on your hand and avoid yawning, yelling, singing, anything that requires the mouth to open wider than it needs to. During rest, be mindful about keeping the jaw slightly ajar so that it isn’t clenched. Also ask your dentist for some good relaxation tips or exercises to help relieve stress.
10. Traditional Treatments
For someone who needs a little bit more than the average home remedy to fix their TMJ disorder, there are also several traditional treatments that a dentist would most likely advise. For starters, there are medications like NSAIDs that treat pain and swelling. Someone who has a problem with clenching their jaw and grinding their teeth might be prescribed a muscle relaxer to relieve stress.
There’s also a night guard or splint that go overtop of the teeth to avoiding grinding them together. “They lessen the effects of clenching or grinding and correct your bite by putting your teeth in a more correct position,” writes WebMD. The only real difference between a night guard and splint is that one is worn all the time and the other is only worn at night. Lastly, WebMD says that a dentist could do some work on your teeth to help relieve the pain by replacing missing teeth or using crowns, bridges, or braces to correct a bite problem.
11. Other Treatments
If none of the above treatments seem to work, then a doctor might suggest any of the following. First up, there’s transcutaneous electrical nerve stimulation (TENS). This is a therapy that uses low-level electrical currents to relax the jaw and relieve pain. This treatment can easily be offered at a doctors office or even at home. WebMD also lists an ultrasound that applies deep heat to the joint to relieve soreness and improve mobility. As well as trigger-point injections which is basically pain medication that is injected into the affected area or “trigger points” to offer relief. Lastly, there is radio wave therapy which uses stimulation to increase blood flow and ease pain or low-level laser therapy.
12. Surgery
Surgery is the last resort for patients with a TMJ disorder because WebMD points out, once it’s done, it can’t be reversed. If a dentist is recommending surgery, be sure to seek out a few other opinions — just in case! Let’s talk through the three different types of surgery available for temporomandibular joint disorder (TMD). First there’s arthrocentesis. WebMD describes it as the most minor of all the surgeries on this list and can be performed by a dentist. This surgery is for someone who doesn’t have a history of TMJ, but suffers from a locked jaw. The procedure basically involves a dentist inserting needles into the joint and washing it out. Then he or she will use a tool to get rid of any damaged tissue or help dislodge a disc that may be stuck in the joint which is what is causing the locked jaw.
The second option for surgery is called arthroscopy which is performed with an arthroscope which allows a doctor to see inside the joint. After receiving a general anesthesia, “the doctor will make a small cut in front of your ear and insert the tool. It’ll be hooked up to a video screen, so he can examine your joint and the area around it. He may remove inflamed tissue or realign the disc or joint.” While this surgery is viewed as minimally invasive, it will leave a small scar. The last option is open-joint surgery which is only an option for people who’s jaw joint is worn down, they have tumors on their joint, or it’s scarred and full of bone chips. This surgery is the most invasive with a high risk of scarring and nerve damage, says WebMD.