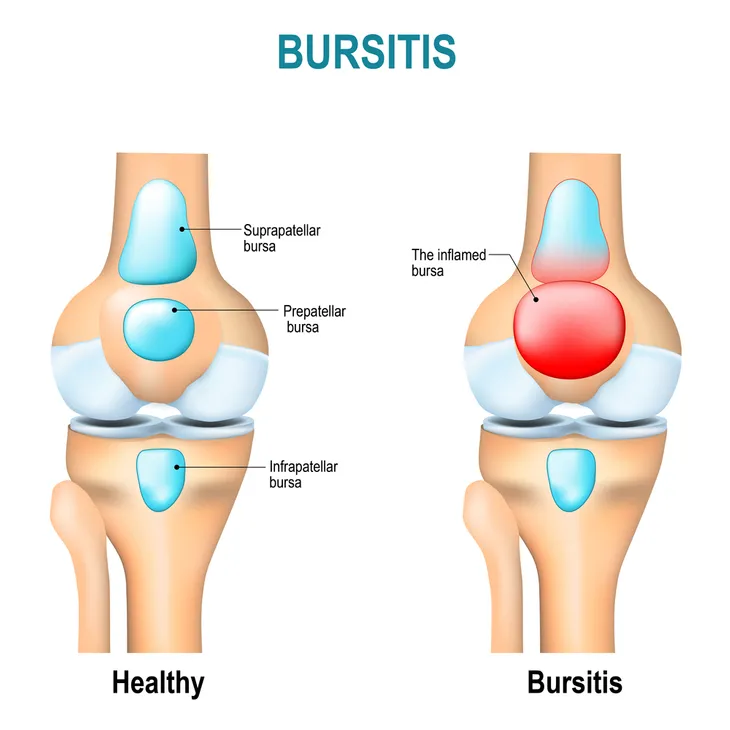
Normally, bursa (sacs of fluid) located around your body serve the purpose of preventing pain by reducing friction between your moving parts. They act as cushions between bones, tendons, and muscles. However, sometimes these bursa can do the opposite. If they become inflamed, they can cause some serious issues.
Whether it’s from repetitive movement or even not moving around for long periods of time, bursitis can occur. Let’s take a closer look at what causes bursitis and what you can do about it.
It Can Be More Than Just Pain
WebMD explains that, while pain that “might build up slowly or be sudden and severe” is the biggest marker of bursitis, there are other signs as well. For example, says the source, you may notice your joints are stiff and swollen along with telltale redness.
The source says there could be symptoms that warrant more immediate medical care. They include a fever of more than 102-F, as well as “general illness” or having trouble moving the particular joint. It most commonly pops up in the elbows, shoulders, hips, knees, heels, buttocks or thighs.
It Can Be Mistaken For Arthritis or Tendinitis
The Cleveland Clinic notes that while both arthritis and bursitis can make the joints feel painful, arthritis usually is the result of “normal wear and tear” on cartilage that is permanent. Bursitis is short-term, unless under repetitive stress.
Meanwhile, tendinitis is inflammation of a tendon that connects bones to muscles, while bursitis (as we’ve noted) is specifically inflammation of a bursa. However, the source explains it’s possible to have both bursitis and tendonitis simultaneously, and tests can sort out this dilemma.
Certain Activities Can Increase Risk
While getting regular exercise is an important part of your overall health, if you’re over 40 you might be more susceptible to bursitis from particular activities, adds WebMD. The source says these “high-risk” activities that could cause the painful condition include gardening, shoveling, or even playing golf or tennis.
The same source notes that being in the same position “the wrong way” for an extended period of time or not adequately stretching before engaging in physical activity can also be risk factors.
There are Different Types
Healthline explains there are actually several types of bursitis. Some of them can be chronic, while others can suddenly appear out of nowhere. Each type of bursitis refers to a different part of the body that is affected.
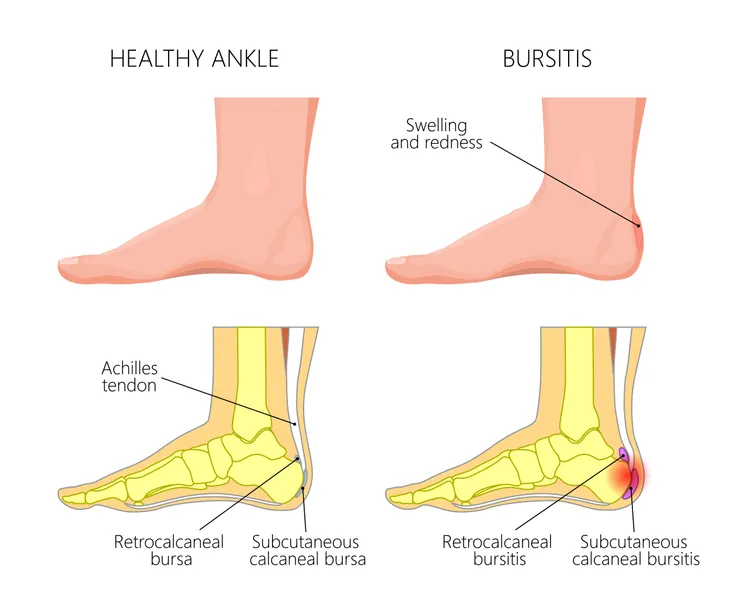
For example, Healthline notes that prepatellar bursitis affects the kneecaps, while olecranon bursitis occurs around your elbows. Meanwhile, trochanteric bursitis occurs in the hips, and retrocalcaneal bursitis can cause discomfort and swelling in your heels. The type that causes redness and fever is known as infectious bursitis.
There Are Varying Triggers For Each Type
Healthline notes the most common reason for bursitis is an injury affecting the bursa (there are 150-plus in the body.) However, when it comes to prepatellar bursitis, causes can include playing sports or standing for long periods of time, adds the source. Olecranon bursitis can be caused by “repeatedly resting your elbows on hard surfaces” and an injury to the elbow, as well as gout.
Meanwhile, trochanteric bursitis can be triggered by lying on your hips for extended periods of time or from incorrect posture while both sitting and standing. Retrocalcaneal bursitis is generally from running and jumping activities, especially if your shoes are too tight in the heel. Infectious bursitis is an infection from bacteria that might be from a surface wound, although other infections can spread to the bursa via the bloodstream, notes the source.
How Bursitis is Diagnosed
Healthline notes that bursitis can often be pinpointed by a physical exam. However, health practitioners can go beyond this step and use medical imaging to get a better look at the affected area, as well as taking blood and tissue samples.
In the case of infectious bursitis that’s limited to a joint, a type of biopsy called needle aspiration is most often used. In other types of bursitis (more specifically olecranon bursitis), needle aspiration may increase “risk of secondary infection” due to moving it from the skin’s surface into a bursa, explains the source. In this case, antibiotics might be prescribed first.
How To Treat Bursitis
The Cleveland Clinic explains the best way to deal with bursitis is actually rest to allow healing, while avoiding the activity that has caused the flare-up. However, along with rest, there are ways to deal with the discomfort, such as icing the area (if it was caused by an injury and not repetitive motion), as well as taking over-the-counter medications to deal with swelling, such as ibuprofen (Advil).
Other approaches, including keeping the injured area elevated or wearing a splint or brace, can prevent the joint from moving around. However, you may need “advanced treatment” that includes antibiotics, physical therapy, or an injection of steroids to quickly relieve pain and swelling. The source notes that, if these approaches don’t resolve the issue, you may need bursa repair surgery after 6-months to a year.
How To Prevent Bursitis
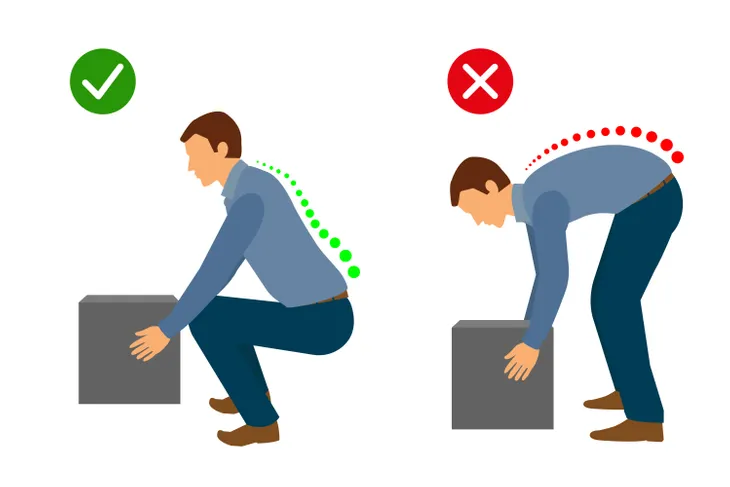
The Mayo Clinic says, “not all types of bursitis can be prevented,” but there are certain approaches you can take to minimize risk. For example, if you have to be on your knees often (e.g., for gardening or work), use knee pads. The source also urges individuals to take breaks often when doing repetitive tasks and using carts instead of trying to move heavy loads that can affect bursae in the shoulders.
If you do have to lift things manually, make sure you bend your knees to not put undue stress on the hip bursae. While exercising is good for “strengthening your muscles and can help protect the affected joint,” it’s important to properly warm-up and stretch before exercising to prevent injury.