Osteoarthritis (OA), also known as degenerative arthritis, degenerative joint disease, and wear-and-tear arthritis, is the most chronic joint condition, says Healthline. It’s also the leading cause of disability, affecting over 30 million Americans.
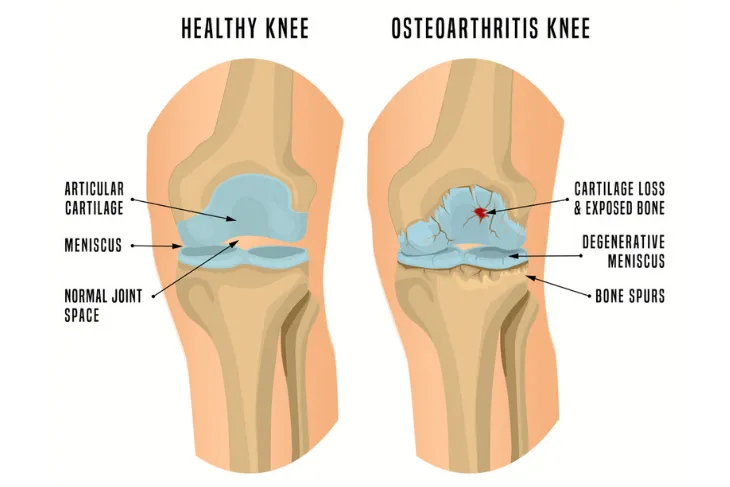
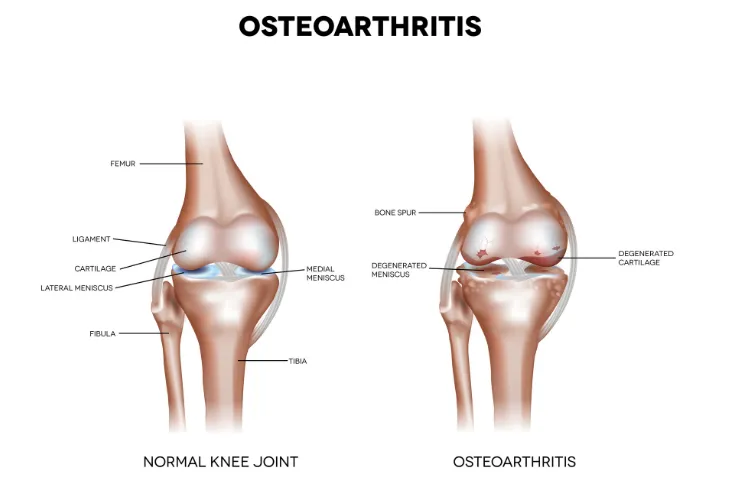
OA is a disease that causes the cartilage in the affected joint to break down. This causes the bones to rub together, leading to pain, stiffness, and a variety of other unpleasant symptoms that we’ll uncover in this article. If you experience one or more of these symptoms, you should book an appointment with your doctor to determine if osteoarthritis or another disease or injury is the underlying problem.
Joint Pain
The most common symptom of osteoarthritis is a pain in the affected joint. It’s also the most noticeable symptom.
Another sign to be on the lookout for is referred pain. This means the pain can be referred to other parts of your body. Arthritis Health says, “For example, hip osteoarthritis may lead to knee pain.”
Joint Stiffness
Another common symptom of osteoarthritis is joint stiffness. This symptom occurs usually after an extended period of inactivity, such as a long car ride, a flight, or even sitting on the couch watching television.
Joint stiffness is also most noticeable in the morning, after laying in bed for hours. The good news is, your joint stiffness will often go away after light activity such as walking around. The movement will help warm up your joints and in turn, reduce stiffness.
Loss of Range of Motion in Your Joints
Joint pain and stiffness aren’t the only symptoms you’ll experience. You may also begin to lose range of motion in your joints too.
Over time as the disease progresses, your joints can become less flexible. This can be caused by bone spurs as well as other tissue changes in your joints.
Loss of Function
Not only can you lose range of motion in your joints but another telling sign of osteoarthritis is loss of function of that joint entirely. The joint may lock up or it may be unable to handle the strain.
For example, if you have arthritis in your hip, you may develop a limp while walking. Or if you have arthritis in your knees, your knee joint may lock up when you try to bend it.
Bone Spurs
Another common sign of arthritis is bone spurs, also medically known as osteophytes. Bone spurs are caused by friction and pressure in the joint’s bones. The bone is trying to heal itself and grow new tissue which results in bone spurs.
It’s worth noting, most aging adults will develop bone spurs in their later years (around age 50 to 60), and they’re not always a sign of arthritis. Your doctor will be able to see bone spurs on your joints through a variety of imaging tests such as an X-ray, computed tomography (CT) scan, or magnetic resonance imaging (MRI).
Physical Deformity of the Joint
Osteoarthritis can also lead to physical deformity of the joint. This is often caused by bone spurs as well as other changes to the affected area.
If you have arthritis in your hands, the joints in your fingers may become enlarged. Further, if you experience a deformity in your knee from arthritis, it may appear bowlegged, says Arthritis Health.
Grinding Sensation in the Joint
Another telling sign of arthritis is a grinding sensation when you bend the joint. It may be accompanied by a popping sound as you straighten the joint. This can happen when the surface of the joint degenerates.
These sensations and noises are medically known as crepitus. It isn’t always a cause for concern unless you are presenting other symptoms too.
Swelling in the Joint
Swelling can also be a sign of osteoarthritis. It occurs when excess fluid builds up in the joint which is medically known as effusion.
If you’re experiencing moderate to severe swelling in your joints, it may also feel warm. Keep a lookout for these common signs of osteoarthritis and inform your doctor if one or more of them arise.
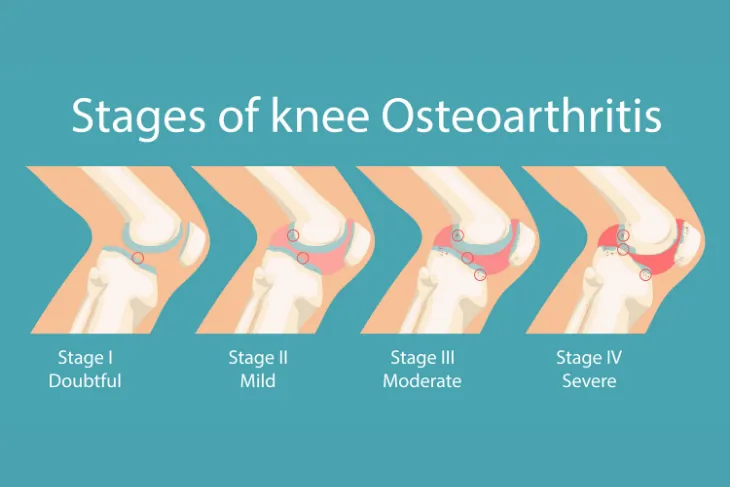
The Four Stages of Osteoarthritis
Along with the common symptoms, the severity of the symptoms can change depending on which stage you’re in.
Osteoarthritis can be broken down into four stages ranging from minor to severe. Let’s take a closer look at what each stage entails.
Stage One: Minor
Stage one is the most minor form of osteoarthritis. During this stage, you’ll begin to develop minor wear and tear on your joints. You also typically don’t experience any pain during this stage.
Your doctor may leave your symptoms untreated, especially if you don’t have a history of osteoarthritis. But if you do begin to develop wear and tear on your joints, they may recommend an exercise routine or supplements to help.
Stage Two: Mild
During stage two, not only will your symptoms begin to advance but signs of osteoarthritis will become more noticeable too. The Orthopaedic Specialty Group says, “This is when X-rays will start to show more noticeable bone spur growths (growths that often develop where bones meet each other in the joint).”
You’ll also begin to notice stiffness in your joint, especially after sitting for long periods. The source also notes, your doctor may suggest a brace or a strict workout routine at this stage.
Stage Three: Moderate
Stage three osteoarthritis is considered moderate. During this stage, your joint will become inflamed due to erosion of the cartilage. This also causes the gap between your bone and the joint to narrow.
The inflammation will also begin causing pain during normal daily activities. Your doctor may recommend over-the-counter (OTC) pain relievers, or prescription medicine to help ease your discomforts.
Stage Four: Severe
Stage four is the most advanced stage of osteoarthritis and it’s also the most painful. In this stage, your cartilage is almost completely eroded. This will trigger an inflammatory response from your joint.
Furthermore, the bone spurs will also multiply which can cause severe pain. Luckily there are various treatment options available, including surgery. Speak with your doctor to determine the right treatment for you.
Risk Factors
Osteoarthritis affects over 32.5 million Americans. More women over 50 have the disease than men the same age, and most over 70 have some symptoms.
Unfortunately, even those in their 20s and 30s can be affected, especially if the following factors exist. Let’s take a look at some of the risk factors for osteoarthritis next!
Genetics and Preexisting Conditions
Osteoarthritis is hereditary. Those born with other bone diseases or genetic traits may be more at risk for developing the disease. Individuals with existing joint abnormalities and those who suffer defective cartilage, may also suffer deterioration of joints and develop osteoarthritis.
Further, certain conditions can also increase your risks, such as gout and rheumatoid arthritis. These conditions can lead to the development of osteoarthritis.
Injury and Repetitive Stress
A prior injury or damage in and around the joints can increase your chances of developing osteoarthritis, especially in the knees and spine.
Joint overuse or an actual repetitive stress injury can also increase your risks. This is common in athletes as well as occupations that require repetitive movements.
Obesity
Obesity is also a risk factor for osteoarthritis. Excessive impact on the joints, particularly on weight-bearing joints like the knees, hips, and spine may lead to the disease.
This is why losing excess weight can help prevent osteoarthritis and joint damage. This can be done by eating a healthy meal plan, staying physically active, managing your stress, and getting enough quality sleep each night.