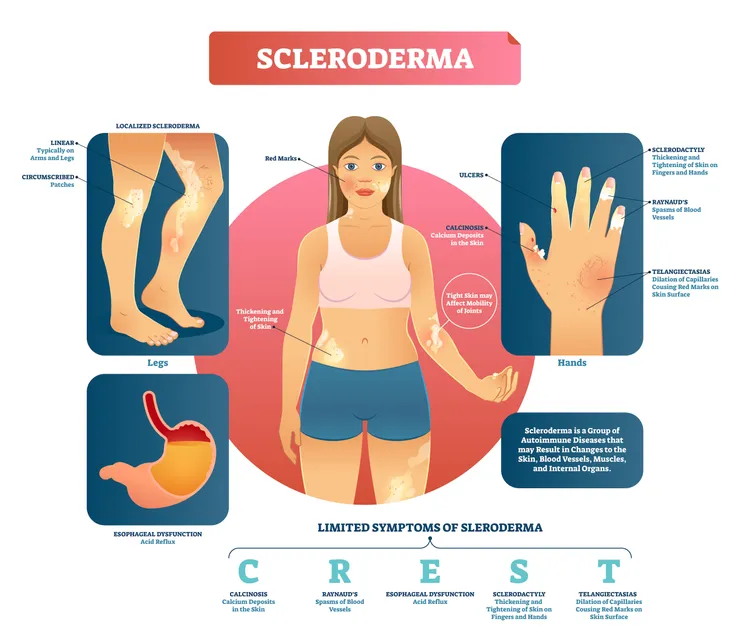
If you’ve never heard of it, scleroderma is an autoimmune and rheumatic disease that can negatively impact the body through the hardening of the skin and underlying connective tissue. It’s also a chronic ailment, meaning it can be hard to completely cure those afflicted by the disease.
Not all scleroderma cases are the same. Some patients will experience only the hardening and tightening of the skin, while others will experience the hardening of connective tissue and even major organs. Left untreated, scleroderma can leave a patient in constant discomfort and pain. That’s why it’s so important to understand the basic rules behind scleroderma.
It’s an Autoimmune Disease
Contrary to popular opinion, an autoimmune disease is not necessarily a disease that attacks the immune system. In actual fact, most autoimmune diseases like scleroderma result in the autoimmune system functioning but not in the interest of the body as a whole. In the case of scleroderma, the pathogenesis is complex but ultimately inflammation leads to increase in scarring cytokines that leads to skin and body changes.
The result: the cells begin to harden and tighten in an effort to repair damage — even though there’s no clear damage to the body or its cells. In turn, this leads to the overproduction of collagen, which can result in general discomfort and even malfunctioning organs.
Every Case is Different
No capable doctor will ever recommend the same treatment regimen to every patient suffering from the same ailment. That’s because every case of a single type of disease can be wildly different and people tend to respond in different ways to each treatment type.
This is especially true for scleroderma, which can be incredibly different from one patient to the next. For some people it may be only a moderate irritation involving slightly harder or tighter skin in isolated parts of the body. But for others it can be a central and problematic part of their lives, leaving them in excruciating pain throughout the day and generally incapable of performing normal daily activities, like caring for children, exercising, or going to work.
It’s Here to Stay
Some ailments can be completely overcome — meaning they can be eradicated entirely from the body with little chance of return. Unfortunately, scleroderma is not one of those ailments. This autoimmune disease is chronic and cannot be completely cured, no matter the choice of treatment or the overall health of the person afflicted. Part of the problem is that there is no known cause for scleroderma.
The good news is that, like many other diseases that can last an entire lifetime, there are many treatment options that can help a patient live a relatively normal lifestyle. These treatments range from physical therapy to medications and even surgery.
Anyone Can Get Scleroderma
Unlike many other diseases where there’s a fairly clear cause for the onset of an illness (such as the emergence of emphysema in a smoker), it’s not known why some people develop scleroderma. While it’s more likely that women and people in their middle age will become scleroderma patients, the old and young can get scleroderma, as can men.
One way to predict the emergence of scleroderma is to focus on families that have seen multiple cases develop. However, even this is complicated, as rarely do families have multiple scleroderma cases; instead, family members may share autoimmune diseases in general. For all these reasons, it can be extremely difficult to predict the onset of scleroderma.
Symptoms Can First Show in Hands
If you think you may be developing scleroderma, there are a few ways to tell. The first way is to examine the fingers, which may become more sensitive to cold temperatures, perhaps even changing color. Fingers can also become stiff and puffy looking.
These changes can spread to the rest of the hands and are the result of the blood vessels gaining excess collagen. Interestingly, changes to the hands and fingers may not just be visible when it’s cold outside; in fact, emotional changes could also impact scleroderma.
A Diagnosis Can Be Tricky
Here’s the thing with scleroderma: it can be tricky to diagnose, especially if the initial symptoms are vague. That’s because the disease tends to develop extremely slowly and may only affect some small parts of the body, such as the fingers, long before spreading. However, seeing the right providers such as rheumatologist or dermatologist is helpful as these are specialists.
This is both a good and bad sign. While it would be idea to make a scleroderma diagnosis early in the disease’s development, the slow growth could also indicate that the scleroderma will not evolve beyond one small part of the body, such as the fingers or a patch of skin. Regardless, it’s important to constantly monitor the condition and be in frequent contact with a physician about it.