- Bowel cancer, sometimes referred to as colorectal cancer, occurs when there is abnormal cell growth anywhere in the colon or rectum.
- A risk factor is something that simply increases the risk of developing cancer. It doesn’t necessarily mean it will happen, but they can lead to a higher chance of developing cancer.
- When it comes to bowel cancer, there are risk factors people cannot change like age and race, as well as those they can which are related to lifestyle (diet, drinking, etc).
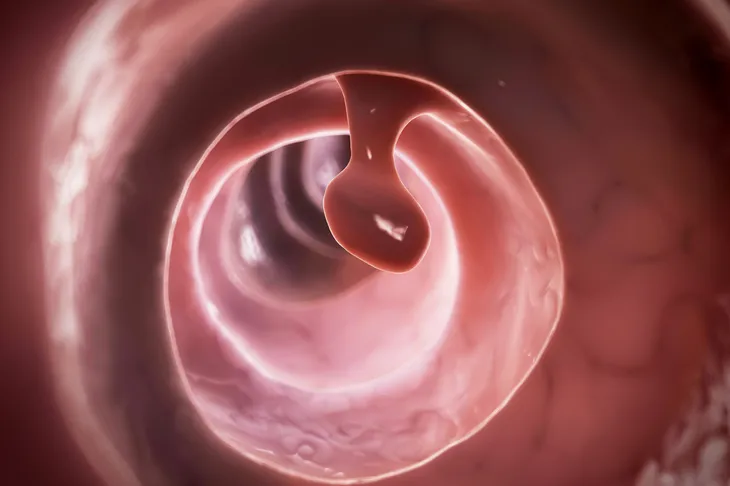
Bowel cancer, sometimes referred to as colorectal cancer, occurs when there is abnormal cell growth anywhere in the colon or rectum. It typically begins in the large intestine (colon), the final part of the digestive tract. For the most part, bowel cancer spreads slower than other cancers and if caught early, it’s often curable, says Colorectal Cancer Canada.
There are many risk factors for bowel cancer. Understanding them can play a key role in prevention and early detection. A risk factor is something that simply increases the risk of developing cancer. It doesn’t necessarily mean it will happen, but they can lead to a higher chance of developing cancer. Unfortunately, sometimes cancer also occurs when people don’t have any risk factors at all.
Here’s a look at the top 12 risk factors for bowel cancer…
Age
Aging is inevitable. As much as we’d like to, we cannot control our age and the fact that we are all getting older each day. Unfortunately, aging is also a risk factor for many cancers, including bowel cancer. While a diagnosis of this cancer can occur at any age, it’s more common among older adults.
According to the Mayo Clinic, most cases of bowel cancer are found in adults over the age of 50. However, the source also notes that doctors have noticed rates of bowel cancer in people under the age of 50 have been increasing and they aren’t sure why.
Family History of Colon Cancer
A person with a family history of bowel cancer means that one or more close blood relatives have been diagnosed with colorectal (bowel) cancer. Sometimes families have more than one case. This can be just a fluke or a result of shared lifestyle factors. It could also be an inherited (hereditary) factor that has been passed from parents to children through genes, or a combination of these factors, writes the Canadian Cancer Society.
In order for family history to play a role, it has to be a first-degree relative. This includes either a parent, sibling, or child. A person’s risk of developing bowel cancer is greater if a first-degree relative has had bowel cancer, warns the Canadian Cancer Society. Rectal cancer is also an increased risk, but the risk is greater with colon or bowel cancer. If there is more than one first-degree relative, that also increases the risk even more. Also, if their diagnosis was before the age of 50.
Medical History
Your personal medical history obviously plays a major role in the amount of risk associated with developing bowel cancer. People who’ve had bowel cancer in the past are more likely to develop it again later in life.
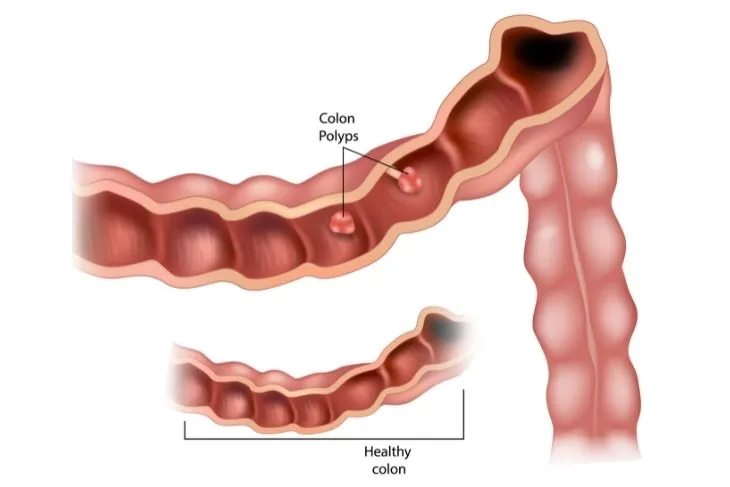
Your risk is also higher if you’ve had noncancerous polyps, says the Mayo Clinic. This is especially true if they’ve had multiple polyps. If colorectal polyps are found in the colon or rectum, even if they are noncancerous, they should be removed because they can become cancerous in the future, warns Johns Hopkins Medicine.
Inherited Syndrome: Familial Adenomatous Polyposis (FAP)
Familial adenomatous polyposis is a rare inherited condition often caused by a mutation of the adenomatous polyposis coli (APC) gene. “FAP causes hundreds to thousands of adenomatous polyps to develop on the inner lining (mucosa) of the colon and rectum,” explains the Canadian Cancer Society. People can develop these polyps early in life, as early as adolescence. If left untreated, the source explains that the majority of people will develop colorectal cancer by the age of 40.
Within FAP is a subtype known as attenuated familiar adenomatous polyposis (AFAP). People with this condition have fewer adenomatous polyps in the colon than people with FAP, explains the Canadian Cancer Society. These polyps tend to develop later in life, as does colorectal cancer.
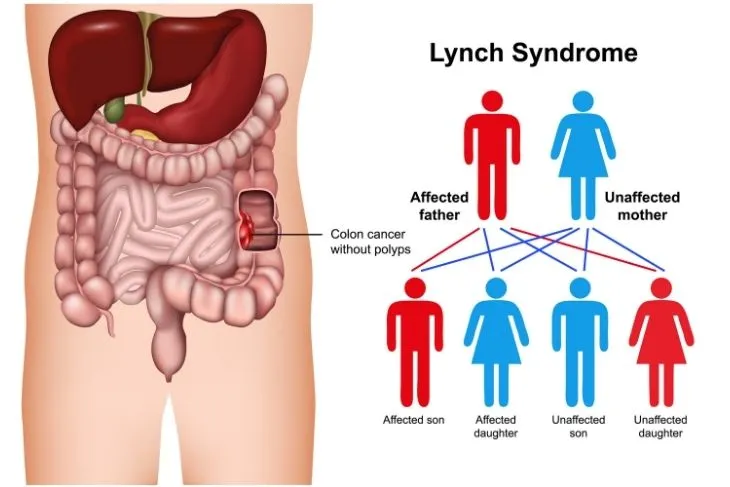
Inherited Syndrome: Lynch Syndrome
Lynch syndrome, also known as hereditary non-polyposis colorectal cancer (HNPCC) is an inherited condition caused by mutations in the genes. These mutations correct mistakes when cells divide and DNA is copied, says the Canadian Cancer Society. “It causes polyps to develop in the lining of the colon, rectum or both, but not as many polyps as in FAP,” writes the source.
It may be suspected that a person has lynch syndrome if they are in their mid-40s and develop colorectal cancer or has a relative who developed colorectal cancer around the same age. The source also adds that it can occurs as two different types.
- Type A (Lynch type 1) increases risk of colorectal cancer only
- Type B (Lynch type 2) increases the risk of colorectal cancer and cancers of the stomach, small intestine, pancreas, kidney, ureter, ovary, uterus, breast, bladder, bile duct, and skin
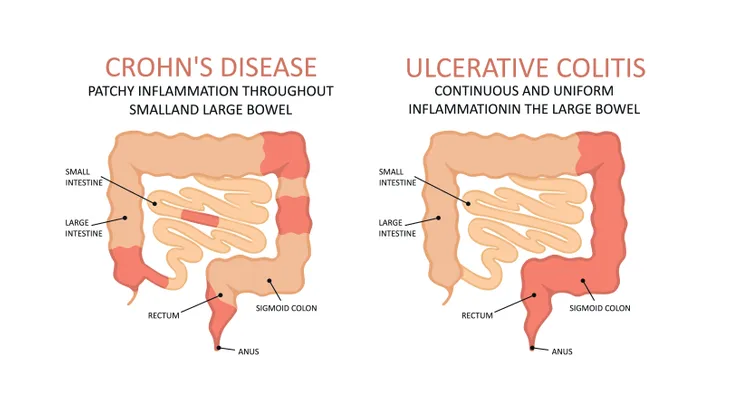
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) is a disease that occurs in the lining of the digestive tract, says the Canadian Cancer Society. It causes the digestive tract to become inflamed and can even lead to sores or bleeding.
The two more common types of IBD are Crohn’s disease and ulcerative colitis. People who suffer from ulcerative colitis have a slightly higher chance of developing bowel cancer than those with Crohn’s disease. However both may cause cellular changes in the bowel as a result of chronic inflammation. “Since these cellular changes can eventually become cancerous, patients with inflammatory bowel disease should receive screening for colon and rectal cancer early and often,” says Johns Hopkins Medicine.
The Canadian Cancer Society adds that the level of risk increases with the length of time a person has IBD and how much of the colon it affects.
Diet
Similar to many other health conditions and issues, diet plays a major role in the risk associated with bowel cancer. The good news is that this is a risk factor that is completely within our control. Our diet can either increase our risk of bowel cancer, or help decrease our risk.
The Mayo Clinic points out that colon and rectal cancer may be linked to a more Western diet. This diet is low in fiber and high in fat and calories. While the research in this area is still a little mixed, some studies have shown that colon cancer is more likely to occur in people who eat more red meat and processed meat.
Sedentary Lifestyle
Regular exercise and movement provides so many great health benefits, such as weight management, disease prevention, and boosting mental health. When it comes to bowel cancer, a more active lifestyle can reduce the risk of developing cancer. You don’t have to become a fitness trainer or workout for an hour everyday. Health experts recommend even just 30 minutes of movement, which includes walking, each day.
Another risk factor that’s tied to this is obesity. People who are overweight have an increased risk of passing away from colon cancer, according to the Mayo Clinic.
Race
Your racial background can affect the probability of whether or not you’ll develop bowel cancer. Similar to age and family history, it’s another risk factor that is completely out of our control. According to Johns Hopkins Medicine, African-Americans and Jewish people of Eastern European descent (Ashkenazi Jews) have a greater risk of developing bowel cancer than people of other races. It’s unclear why this happens.
The Canadian Cancer Society adds that for Jewish people of Eastern European descent, they “tend to have a specific mutation in the APC gene that increases the risk.” This genetic mutation isn’t commonly present in other ethnic groups.
Smoking and Drinking
People who smoke have a higher risk of developing bowel cancer, as well as people who drink heavily. While it’s not realistic for people to stop drinking alcohol entirely, it has been found that moderate to heavy drinking, and even light to moderate drinking can increase the risk of bowel cancer. “Men should limit themselves to two drinks a day and women to one drink a day,” warns Cancer Treatment Centers of America.
A report published by the American Cancer Society said that the International Agency for Research on Cancer can now definitively say that smoking tobacco causes colorectal (bowel) cancer. “About 12-percent of U.S. colorectal cancer cases are caused by current or former smoking,” writes the source.
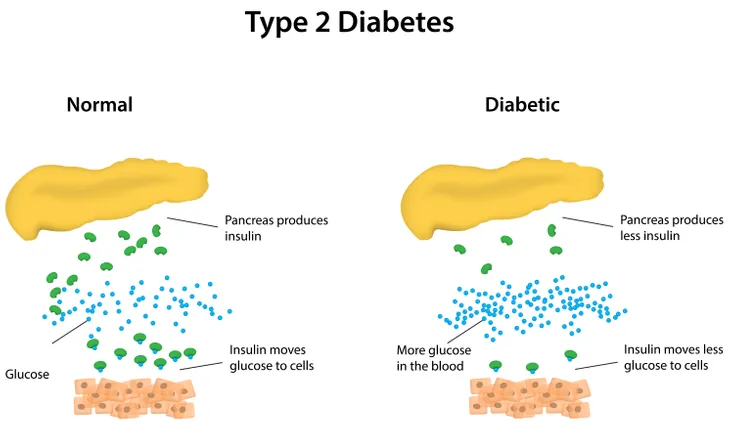
Diabetes
Unfortunately, people who have diabetes or a resistance to the hormone that regulates glucose in the blood are at risk of developing bowel cancer. However, it’s important to note that the risk is primarily associated with type 2 diabetes.
The risk that comes with type 2 diabetes often has to do with a higher level of physical inactivity and being overweight or obese — both of which are risk factors for type 2 diabetes and bowel cancer.
Rare Genetic Conditions
There are several genetic conditions that contribute to a persons level of risk when it comes to developing bowel cancer. Thankfully, all of these conditions are quite rare. Turcot syndrome is a variant of lynch syndrome and FAP. People with this condition may develop polyps in the colon that turn cancerous. MYH-associated polyposis (MAP) occurs due to a mutation in the MUTYH DNA repair gene. People with this condition may develop adenomatous polyps in the inner lining of their colon, says the Canadian Cancer Society.
Another genetic condition that can lead to bowel cancer is juvenile polyposis syndrome. People inherit this condition from a blood relative. It causes polyps call hamartomas, explains the same source. These are usually non-cancerous, but they can turn into cancer.
The Canadian Cancer Society also lists the following genetic conditions as potential risk factors:
- Peutz-Jeghers syndrome
- Hereditary mixed polyposis syndrome (HMPS)
- Cowden syndrome
- Bannayan-Riley-Ruvalcaba syndrome