Peripheral artery disease (PAD), also known as peripheral arterial disease, is a condition that occurs when your arteries are narrowed and can’t carry as much blood from the heart to the outer parts of your body. It most commonly affects the legs and arms, but it can also occur in the stomach and kidneys.
It is serious as untreated PAD can increase your risks of heart attack or stroke. This is why it’s important to know the signs. Here’s everything you should know about PAD including the common symptoms, causes, and treatment options.
Common Signs and Symptoms of PAD
One common sign of PAD is a pain in your calves when exercising or walking. This pain typically goes away with rest. This is called claudication. PAD sufferers may also experience numbness, tingling, or a feeling of pins and needles in the lower legs or feet. Finally, slow healing wounds is another potential sign of PAD.
While this condition affects millions of Americans, Healthline says “many doctors and patients overlook subtle signs of the condition.” Some individuals even dismiss the pain as a sign of aging. But it’s vital that you pay attention to your body and report any changes to your doctor. The source notes that early treatment is important to protect your vascular system.
Advanced Symptoms
As PAD progresses, you may begin to develop other symptoms. For starters, WebMD notes advanced forms of PAD can cause your toes or feet to hurt even while resting. In some cases, it may even disrupt your sleep.
Other advanced symptoms include changes in the color of your legs, fatigue while walking, one leg feeling cooler than the other, and loss of hair on your legs. Other signs include slow toenail growth, pale/blue-looking skin or shiny skin on the legs, and slow healing wounds on your toes and feet.
Who’s at Risk for PAD?
Certain factors can increase your risk of developing PAD. For starters, diabetes is a big risk factor but having a family history of heart disease or being over the age of 50 can also increase your risk.
If you have high cholesterol, high blood pressure, or have had a heart attack or stroke in the past you may also be at risk for PAD. Being overweight or obese and physically inactive are risk factors too. Finally, smoking is another huge contributor which we’ll explain more next.
The Impact of Smoking
WebMD says, “smoking is the single biggest PAD risk factor that is in your control.” The source says your risk of PAD increases by 400-percent if you smoke compared to nonsmokers. What’s more, smokers typically develop symptoms of PAD 10-years earlier than nonsmokers.
Further, smokers have even more risks. They’re twice as likely to require limb amputation, are more likely to pass away after a stroke or heart attack, and often don’t recover as well after some types of heart bypass surgery. Are you convinced that you should quit? To get the support you need, talk to your doctor about quitting.
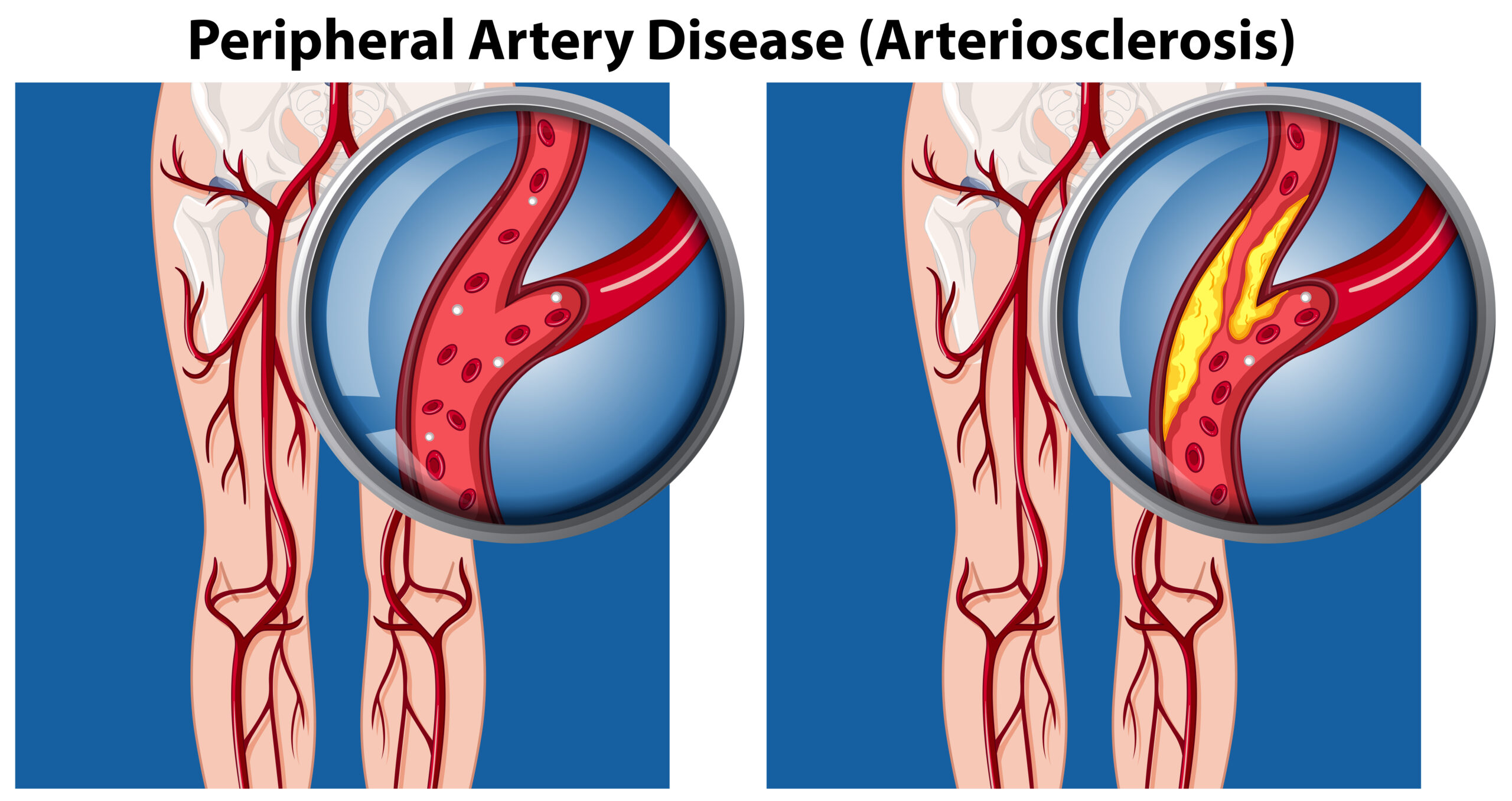
What Causes PAD?
The Mayo Clinic explains PAD is caused by a build-up of plaque in your blood vessel walls, also known as atherosclerosis. The plaque restricts blood flow and oxygen to your legs and feet. Many people associate atherosclerosis with the heart but it’s a disease that can affect arteries throughout your entire body.
Though less common, PAD may also be caused by an injury to your limbs, unusual anatomy of your ligaments or muscles, blood vessel inflammation, or exposure to radiation.
When to See a Doctor
If you develop pain in your leg, especially when you walk, or any of the other common PAD symptoms then you should book an appointment with your doctor. WebMD also advises that you should ask your doctor about PAD if you’re 70-years old or older.
If you’re a smoker, have diabetes, a family history of PAD, or any of the other risk factors for PAD you should also talk to your doctor about it. Early intervention is key.
How Is PAD Diagnosed?
The Centers for Disease Control and Prevention (CDC) explains if your doctor suspects you may have PAD, they will do an ankle-brachial index (ABI). This noninvasive test measures the blood pressure in your ankles and compares it to the blood pressure in your arms. If your blood pressure is lower in your ankles than your arms, you likely have PAD.
In some cases, you may not get a clear diagnosis from an ABI alone. In this case, your doctor may also require imaging tests such as ultrasound, computed tomographic (CT) angiography, or magnetic resonance angiography (MRA).
Complications
While PAD may not seem that serious, WebMD points out, “PAD can be a warning sign because if you have plaque in your legs, you probably have it in other places, too.” One of those other places could be the arteries of your heart, known as coronary artery disease. This greatly increases your risk of a heart attack.
Further, the source points out that you may also have plaque build-up in the arteries going to your kidneys, which is known as renal artery disease. Another commonplace is in the carotid arteries, which are responsible for supplying blood to the brain. If this occurs, you can have an increased risk of a stroke.
PAD and Diabetes
A heart attack and stroke aren’t the only two health problems you have to worry about with PAD. If you have diabetes and PAD, then you’re at a greater risk for developing critical limb ischemia.
Critical limb ischemia is a condition that starts as open sores or infection typically in the foot or leg. However, they don’t heal or go away. This can be serious because in some cases it can lead to amputation of the affected limb.
Treatment: Lifestyle Changes
One way to help manage your symptoms and to prevent your condition from getting worse is making lifestyle adjustments. For starters, your doctor may recommend controlling your cholesterol and blood pressure.
Controlling your blood sugar, especially if you have diabetes, is also important. If you smoke your doctor will recommend that you quit. Finally, your doctor will likely also recommend eating a healthy diet and exercising.
Other Treatment Options
If lifestyle adjustments are not enough for your condition your doctor may recommend other treatment options such as an angioplasty. This is a procedure that uses a catheter (thin tube) to put a small balloon in your artery. Once the balloon is inflated, the plaque will be pushed out to widen the artery and restore blood flow. In some cases, your doctor may put a stent into your artery in order to keep it open and allow blood flow.
In other cases, your doctor may recommend surgery. A procedure known as bypass graft can route your blood flow around the blocked artery. Finally, there are also some medications available that can help manage your symptoms, improve your poor circulation, and other types can help lower your cholesterol, blood pressure, and blood sugar. Your doctor will recommend which treatment option is best for you.
Preventing PAD
Now that we have an understanding of what PAD is and the risks associated with it, you might be wondering how do you prevent it from happening? The CDC says to prevent peripheral artery disease maintain a healthy lifestyle.
The source says engaging in regular physical activity can not only help prevent PAD but can also improve the symptoms if you have it. You should also quit smoking as it increases your risks for PAD and can make your symptoms worse. Finally, if you have high blood pressure, high cholesterol, or diabetes be sure to control your conditions to prevent PAD.