When we hear the word “ulcer” it just gives us a shudder because as most people know, an ulcer is an open sore. There’s nothing nice about that! If you thought that was bad, now think of this, an open sore that is located inside the body…in the stomach. Yikes! This is a peptic ulcer. They can also develop in the first portion of the small intestine, which is called the duodenum. That sounds incredibly painful, and it is. While it’s bad enough that these ulcers can cause pain and discomfort, they can also cause complications, such as internal bleeding, obstructions, and perforations (or holes) in the digestive system, that require immediate medical attention.
To help avoid any serious complications from an ulcer, we’ve created an informative list of everything a person should know about peptic ulcers, including the symptoms, causes, and possible treatments. Take a look…
What are Peptic Ulcers?
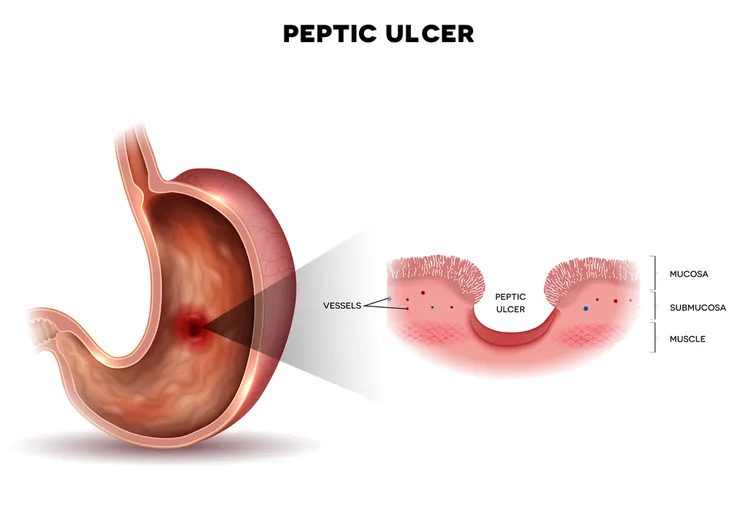
As we’ve already mentioned, an ulcer is an open sore. So, what’s a peptic ulcer? Well a peptic ulcer is one that develops inside the stomach, but they can also be found in the small intestine. In summary, there are two different types of peptic ulcers: gastric ulcers which develop in the lining of the stomach, and duodenal ulcers which develop in the first portion of the small intestine (duodenum), says WebMD.
A peptic ulcer develops when the “stomach acids etch away your digestive tract’s protective layer of mucus,” writes WebMD. Not surprisingly, they often result in a great deal of pain and discomfort, but what’s scary is that they don’t always present any symptoms which means a person could have them and not be aware of it. In severe cases, they can lead to internal bleeding, perforation or obstruction of the digestive system.
Symptoms of Peptic Ulcers
The most obvious symptom of peptic ulcers is pain and discomfort, which we’ve already mentioned. The pain will be located in the abdomen, typically the upper abdomen, but it can also travel to the back. The degree to which the pain is felt can vary. Very Well Health says it can be “dull, burning, or gnawing,” and less commonly, “intense or stabbing.”
There are several other symptoms such as loss of appetite, discomfort and bloating, weight loss, indigestion, chronic nausea alongside discomfort with eating, frequent burping, diarrhea, blood in the stool, as well as fatigue or weakness (stems from malnutrition or internal bleeding), that can be caused by ulcers.
Symptoms and Eating
Some of the symptoms are in relation to eating, digesting food, or an empty stomach. For example, Very Well Health says that some people will experience pain when their stomach is empty. The symptoms could also get better after you’ve eaten something, only to return with a vengeance about an hour later. You’d think that this would cause people to overeat so that they can get some relief, but according to Very Well Health people with peptic ulcers tend to not eat as much because they also suffer from “nausea and discomfort can squash appetite or the desire to eat.” Also, certain foods such as fatty foods will make the symptoms worse, while other foods will elicit no symptoms
The source also notes that peptic ulcers can develop as a result of other conditions, such as gastroesophageal reflux disease (GERD), chronic dyspepsia, gallbladder disease, liver disease, and gastrointestinal infections. Seek out a doctor to help pinpoint what the exact cause of the symptoms are.
When to See a Doctor
It can be hard to know when a health condition has gone beyond the norm and become serious. Healthcare professionals like to avoid overcrowding emergency rooms, doctor offices, and hospitals, so it’s important to be informed on what is considered a serious health complication. The Mayo Clinic advises seeking immediate care if any of the more severe symptoms listed above, such as vomiting blood, trouble breathing, dizziness, nausea, unexplained weight loss, or appetite changes, occur. Another source, Very Well Health, says symptoms such as pain in the back, pain that doesn’t go away, weakness and fatigue, also indicate that you should make an appointment with your doctor.
If any of the symptoms above persist for longer than a week, you should make an appointment with your doctor. This way you can determine whether the problem is a peptic ulcer and receive treatment, which is especially important if you’re also experiencing more serious complications (such as internal bleeding).
Cause: Bacteria
The bacteria that causes ulcers is called Helicobacter pylori (H. pylori) and WebMD says most people carry it in their digestive system, in fact nearly half of people have it. Obviously most of these people are not affected by it in the form of ulcers, but a small percentage of people will develop ulcers as the bacteria “can raise the amount of acid, break down the protective mucus layer, and irritate the digestive tract.” The source also states that experts haven’t been able to figure out how this bacteria spreads, but it’s likely from close contact, such as kissing, or through unclean food and water.
Cause: Certain Medication
Certain medications can put the body at risk for other complications. For example, someone who’s been taking aspirin on a regular basis is more likely to develop a peptic ulcer. WebMD elaborates that this is also true for other medications such as ibuprofen, naproxen, and other nonsteroidal anti-inflammatory drugs (NSAIDs). For example, “NSAIDs block your body from making a chemical that helps protect the inner walls of your stomach and small intestine from stomach acid,” writes WebMD. Don’t fret if you’ve been taking the pain medication acetaminophen, because WebMD says this hasn’t been linked to causing peptic ulcers.
Other Causes
Other causes of peptic ulcers are medications such as “steroids, anticoagulants, selective serotonin reuptake inhibitors (SSRIs), alendronate (Fosamax) and risedronate (Actonel), [which] can greatly increase the chance of developing ulcers,” explains Mayo Clinic. Healthline also lists radiation therapy and stomach cancer as potential causes of peptic ulcers.
Risk Factors
Other common causes of peptic ulcers, or at least puts people at a higher risk of developing them, are smoking and drinking alcohol. WebMD also notes that experts once thought that eating a lot of spicy food and stress cause ulcers, but that has been found to be not be true. The only thing that stress and spicy food will do is make an already existing ulcer worse.
Complications
We’ve already touched on some of the severe complications that can arise from peptic ulcers, but we’ll go into more details here. The first major complication is internal bleeding. The Mayo Clinic explains that this blood loss can happen closely over time and lead to anemia, or if it’s more severe, it could require hospitalization and even a blood transfusion. Someone who is suffering from a peptic ulcer and is experiencing internal bleeding will notice their stools, as well as their vomit (if applicable), are extremely dark (black or bloody).
Another potential complication is infection as the ulcer “eats a hole through the wall of the stomach or small intestine, putting you at risk of serious infection of your abdominal cavity (peritonitis),” writes the source. Lastly, a peptic ulcer can cause an obstruction, which clogs the digestive system by not letting food pass through. This results in the patient feeling full on a regular basis, losing weight, or frequently vomiting due to the inflammation.
Diagnosis
Because a peptic ulcer is located within the body in either the stomach or small intestine, it’s impossible to determine if it’s the problem without performing either an upper endoscopy or an upper gastrointestinal (GI) series. An upper endoscopy is when “the doctor inserts a long tube with a camera down your throat and into your stomach and small intestine to examine the area of ulcers,” explains Healthline. This tool also allows the doctor to remove samples that can be further examined. This test is not advised for people who are at a higher risk for stomach cancer, over the age of 45, have difficulty breathing, suffer from anemia, or who have experienced weight loss, or GI bleeding.
The other test referred to as an upper GI series (or “barium swallow”) is more common. This procedure requires patients to drink a thick liquid called barium to help clear the intestines, and then “a technician will take an X-ray of your stomach, esophagus, and small intestine. The liquid will make it possible for your doctor to view and treat the ulcer.” Healthline also notes that because peptic ulcers can be caused by the bacteria H. pylori, the doctor might run a test to check for its presence in the stomach.
Treatment
Once a peptic ulcer is diagnosed, the next step is to determine how to proceed with treatment. This will depend on what the cause of the ulcer is. If it’s due to the bacteria H. pylori, the method of treatment is typically “triple therapy” with two antibiotic medications to kill the infection and a proton pump inhibitor (PPI) that will reduce the amount of acid your stomach produces. These medications are the most common form of treatment, but they can cause diarrhea and an upset stomach. If the symptoms don’t go away in 2-weeks, please book another visit with your doctor.
However, not all peptic ulcers are due to this bacteria, so another option is an “over-the-counter PPI (such as Prilosec or Prevacid) for up to eight weeks to reduce stomach acid and help your ulcer heal,” says Healthline. Your doctor could also prescribe ranitidine (Zantac) or famotidine (Pepcid), which work as acid blockers to reduce the amount of stomach acid and hopefully relieve pain.
Prevention
Peptic ulcers are a scary thing, but luckily, there are things a person can do to protect themselves and prevent an ulcer from developing. Because there is some belief that the H. pylori bacteria spreads through close contact, the Mayo Clinic advises people practice extra caution when it comes to protecting themselves from infection. This means washing hands frequently and being careful to not eat foods that have not been cooked properly.
Another way to protect and prevent ulcers is to monitor consumption of pain relievers. Only use them when necessary and avoid using them on a regular basis. If you’re having trouble with this, consult a doctor to find the lowest dosage that relieves your pain, or better yet, ask for an alternate pain reliever, if one is available. The Mayo Clinic notes patients should also avoid drinking alcohol when on pain-relieving medication.