Pan-ulcerative colitis (also known as pancolitis) is a condition that affects the entire large intestine. IBDRelief notes that this condition falls under the category of inflammatory bowel diseases (IBD), and is chronic and incurable.
However, while pancolitis can be difficult to deal with, there are some treatment options available to help improve quality of life. There are also some lifestyle adjustments that can be made to help mitigate the symptoms. Read on to learn more about the topic…
What Are the Symptoms of Pancolitis?
Medical News Today explains that there are main and secondary symptoms of pancolitis to expect. For example, the biggest symptoms are usually recurring diarrhea that may have blood or mucus, notes the source.
There’s often also abdominal cramping, and an “urgent” feeling that you have to go to the bathroom often. Less common symptoms of this form of UC include weight loss, fatigue, loss of appetite, and in some cases, a fever or night sweats.
Flare-Ups Can Occur
While some of the symptoms of pancolitis can be mild for some time, flare-ups/relapses may occur. Medical News Today explains “if a person has not experienced symptoms of pancolitis for a significant period and then they suddenly return, it is known as a flare-up or relapse.”
The source also notes that a flare-up can also cause symptoms in other areas of the body. For example, the individual may experience painful or swollen joints or skin, shortness of breath, fast or irregular heartbeat, ulcers in the mouth, irritated red eyes, or a high temperature.
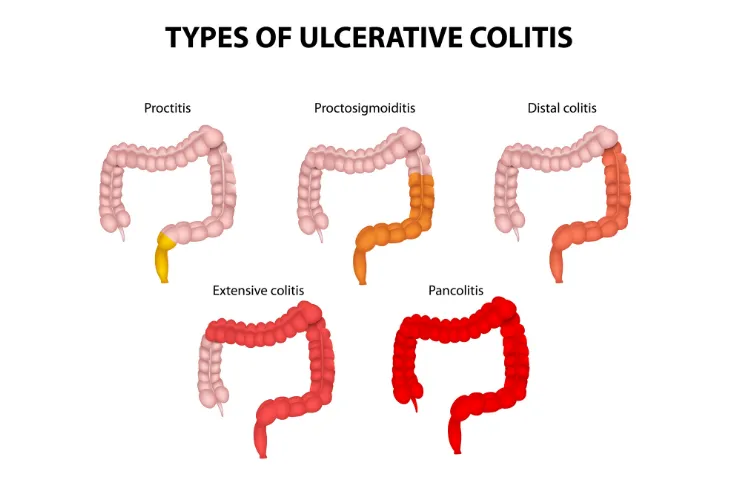
Ulcerative Colitis vs. Pancolitis
Ulcerative colitis, or UC for short, causes irritation and inflammation in the large intestine that leads to a range of symptoms from pain to anemia. Some medical experts regard it as an autoimmune disease, as the symptoms are caused by an overactive immune response.
IBDRelief notes that pancolitis is a form of UC. While UC causes inflammation in various parts of the colon depending on the type, pancolitis affects the entire intestine. The source notes that often patients with pancolitis begin by experiencing another form of UC, such as proctitis that only affects the rectum. The source adds that about 20-percent of UC patients have pancolitis.
Are There Any Complications of Pancolitis?
IBDRelief explains there are some bigger risks associated with having pancolitis. For example, it notes that those with this UC have a greater chance of bowel cancer.
There’s also something called “toxic megacolon” that happens when inflammation of the bowel spikes, which can lead to dehydration and fever. The colon can also rupture in some cases.
 Prostock-studio / Shutterstock
Prostock-studio / ShutterstockOther Complications
IBDRelief also says that there’s a more severe form of pancolitis called fulminant colitis, which is rare. However, those who have this form experience protracted diarrhea (lasting 2-weeks or more with the presence of blood) as well as possible “shock.”
What Causes It?
Medical News Today confirms that UC in general is an autoimmune disease. While the exact cause of this group of IBDs is not yet fully understood, the source says that the medical community has determined some factors that might increase the risk of developing it.
For example, it says scientists suspect that genetics may play a role in developing pancolitis and other UCs. It also lists “an abnormal reaction from the digestive system to bacteria in the intestine” as another possibility. It also makes note of “unknown triggers” that include viruses or diet.
When to See a Doctor
Healthline notes that some of the symptoms of pancolitis (such as pain and cramping) might actually be caused by gas or even food poisoning. However, if that’s the case, then the symptoms will be temporary and will clear up.
The source says if you notice blood in your stool, have diarrhea that lasts more than 2-days (that can’t be helped with medicine), you’re running a fever, or you’re experiencing severe abdominal pain, then it’s time to get yourself to a doctor as soon as you can.
How Is Pancolitis Diagnosed?
Medical News Today says that a doctor will assess your symptoms and overall health during the visit. They may also take stool or blood samples to check for infection or inflammation.
There are other methods that a doctor may use to diagnose the disease. They include medical imaging tests such as computed tomography (CT) scans that can rule out other conditions. You might also be asked to have a colonoscopy, which involves inserting a flexible tube equipped with a camera to have a better look inside.
There Are Medications Available
Medical News Today explains there are 4-types of medications that will be considered for treating pancolitis. They include aminosalicylates (ASAs) that are designed to reduce inflammation, in pill form that can be taken orally or as a rectal suppository. This option is chosen for mild to moderate cases, it adds.
The source also says corticosteroids can also help reduce inflammation. Meanwhile, there are immunomodulators that calm the immune system, which are usually given if there’s a flare-up of symptoms. Biologics are another option and can target “specific components of the immune system involved in inflammation,” it adds.
Surgery Is an Option
If medications aren’t working as they should, your medical team might turn to surgery. Medical News Today explains that often, the entire colon will be removed to prevent any chance of the condition returning. However, the patient will need to pass waste through a hole in the abdomen into a bag (ileostomy) following this procedure.
However, the need for a bag may not be permanent. The source points out that a second surgery can be considered later on to create something called an “ileoanal pouch,” which connects the small intestine to the anus to pass waste as before.
Lifestyle Adjustments Might Help
Healthline lists some possible non-medical approaches to managing your symptoms, while also ensuring you get enough nutrients. It notes you should keep a food diary to help you figure out which foods to avoid – and dairy is one thing you should be reducing.
The source also suggests avoiding carbonated and caffeinated drinks and reducing your intake of insoluble fiber (from sources such as bran, whole grains, and some vegetables). Try to drink about eight glasses of water per day and consider multivitamins as a supplement, the source notes.
What Is the Outlook?
Although there is no cure, those with pancolitis can experience periods of remission when the symptoms don’t impact daily life, explains Medical News Today. However, if the signs return, you might have to lower your daily activities to help manage them.
The source also explains that there can be emotional issues attached to this chronic condition. That’s why it’s important to seek out support from healthcare professionals, as well as family and friends. There are also online UC support groups you can join.