You’ve likely heard of osteoporosis, which is a disease that weakens the bones so severely that it can cause the bones to break, but not many people have heard of osteomalacia, which is a disease that keeps your bones from hardening as they should.
There’s a lot more to know about this disease and the risks that are involved. To better understand it, let’s uncover everything there is to know about osteomalacia, including the symptoms, causes, and treatment options available.
What Is Osteomalacia?
Osteomalacia means “soft bones,” and it’s a disorder of decreased mineralization. This means the bone breaks down faster than it can reform.
This disease can affect individuals of all ages, because our bones continuously go through a process called bone turnover. Medical News Today says, “Bone turnover is when the body reabsorbs the old tissue and forms new bone tissue, starting with the softer inner layer that comprises collagen.”
When an individual has osteomalacia, he or she will also experience another process called decreased mineralization, which means the outer shell of bone doesn’t form fully and leaves the collagen soft and unprotected.
The Difference Between Osteomalacia, Rickets, and Osteoporosis
There are a couple of other bone diseases that seem similar to osteomalacia, including rickets and osteoporosis. Let’s explore their differences.
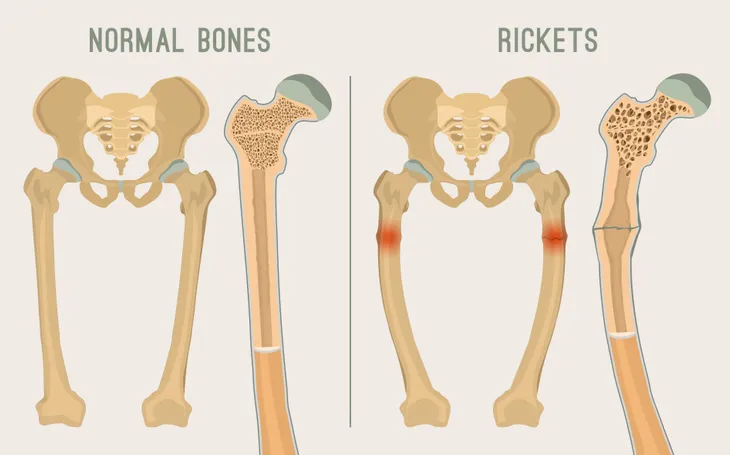
First, the biggest difference between osteomalacia and rickets is the age group it affects. Rickets is a disease that only develops in children because their bones are still growing, and it can cause deformed bones. Whereas, osteomalacia can develop in individuals of all ages.
In contrast, osteoporosis is a disease that causes the bones to become porous and brittle, which increases the risk of broken bones (fractures). The biggest difference here is that osteomalacia causes the bones to become soft and osteoporosis causes bone loss.
Symptoms of Osteomalacia
Osteomalacia sufferers may experience muscle weakness due to problems in the area where your muscle is attached to the bone. However, the most common symptom of osteomalacia is bones that fracture easily.
Others may also develop a waddling gait or bone pain, particularly in the hips. The pain is known to spread from the hips to the lower back, legs, pelvis, and ribs.
Additional Symptoms
Osteomalacia sufferers who have low levels of calcium in their blood may also experience additional symptoms. This includes irregular heart rhythms and spasms in the hands and feet.
Numbness in your arms and legs, as well as around your mouth, is also common if calcium levels are low.
When to See a Doctor
If you notice any symptoms of osteomalacia it’s imperative that you see your doctor. Leaving this disorder untreated can cause serious complications, including bones that can fracture easily.
Book an appointment with your doctor and explain your symptoms. He or she will be able to make a diagnosis and determine the right treatment for you.
What Causes Osteomalacia?
There are a few things that can cause osteomalacia, but vitamin D deficiency is the most common. Vitamin D is an essential nutrient that helps your body absorb calcium, and calcium is essential for building and maintaining strong bones.
Furthermore, Healthline states, “Vitamin D also helps maintain calcium and phosphate levels to help your bones form properly.” The good news is, you can absorb vitamin D through the skin from exposure to the sun’s ultraviolet (UV) rays, but it can also be absorbed from vitamin D-rich foods. That said, some factors can interfere with how your body absorbs vitamin D. Let’s look at these next.
Causes of Vitamin D Deficiency
If you are vitamin D deficient, then your body won’t be able to process the calcium your bones require to stay strong and healthy. A poor diet, lack of sun exposure, and intestinal issues can all be causes of vitamin D deficiency.
Some individuals may have a hard time absorbing vitamin D if they have a surgery that removes part of the stomach or small intestine. Other conditions such as celiac disease, some types of cancer, and kidney and liver disorders can also interfere with how your body absorbs vitamin D.
Other Causes of Osteomalacia
Healthline also states that phosphate depletion can lead to osteomalacia. This usually happens when your diet doesn’t include any phosphorus-rich foods.
Finally, some medications such as phenytoin and phenobarbital (which are used to treat seizures), may also cause osteomalacia.
Diagnosing Osteomalacia: Blood Test
To diagnose osteomalacia, your doctor may request a blood test. They’ll be on the lookout for low levels of vitamin D, calcium, and phosphorus, which may indicate you have osteomalacia.
Your doctor may also check your alkaline phosphatase isoenzymes or parathyroid hormone levels. High levels of either may indicate you have osteomalacia.
Diagnosing Osteomalacia: X-Rays
Another way to diagnose osteomalacia is through X-rays and other imaging tests. These tests will be able to show your doctor if you have any small cracks (known as Looser’s transformation zones) in your bones.
Finally, if a blood test or X-ray isn’t enough to diagnose this condition, your doctor may need to do a bone biopsy. To do this, they will insert a small needle into your bone to take a small sample.
Treatment Options
The good news is, if detected early, the only treatment you may need is to take oral supplements of vitamin D, calcium, and/or phosphate. Vitamin D can also be absorbed by spending time outdoors in the sunlight and in rare cases, you may need to take the supplement intravenously through a vein in your arm.
Furthermore, if there’s an underlying condition causing your vitamin D deficiency, it will need to be treated as well. Finally, children who experience a severe case of osteomalacia or rickets may need to have surgery or wear braces in order to correct the bone deformation.
The Risks of Leaving Osteomalacia Untreated
Treating osteomalacia is crucial. If left untreated, it may lead to broken bones and even severe deformity. If you suspect you have osteomalacia or are at risk for developing it, make sure you speak with your doctor.
Thankfully, there are treatments available that can help you manage the condition. With the right treatment, you may see improvement in just a few weeks but it takes about 6-months for your bones to fully heal.