It may sound like something out of a science fiction movie, but the fact is that molluscum contagiosum is a fairly common skin infection that presents as raised bumps or lesions. It is most commonly found in children from the ages 1 to 10-years, according to the CDC, but can affect the older population too.
While it’s typically not considered dangerous or painful, it can be distressing for the patient and last for a long time. Luckily, there are treatments for the more prominent cases, and the problem often disappears on its own if a person’s immune system in functioning optimally. Here’s what you need to know about it…
What is Molluscum Contagiosum?
The CDC explains the skin condition is caused by a poxvirus, the same virus that once caused smallpox that has been eradicated. The molluscum contagiosum virus itself is benign (not cancerous), adds the source. It is transmitted by coming in contact with someone who is infected, or by touching an infected object.
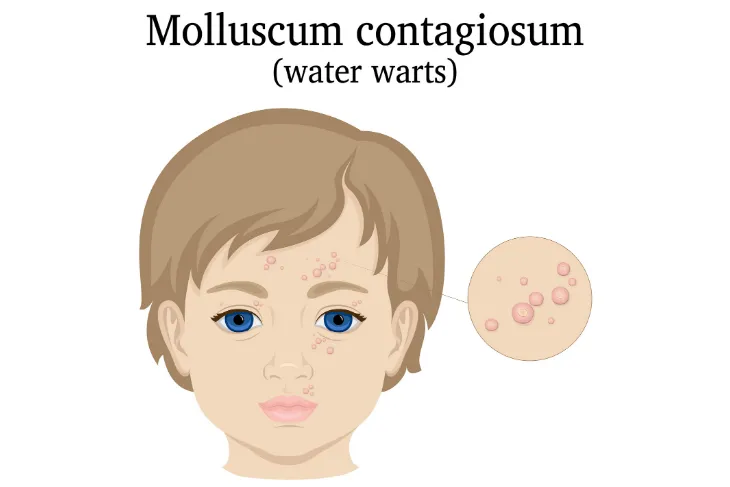
The source also explains that the mollusca – the medical term for the skin lesions caused by the virus – are tiny but can be as large as a pencil eraser, and can show up in multiple places on the body including the face, it adds. The methods of transmission can change depending on age group.
What are The Symptoms?
Healthline explains the bumps associated with molluscum contagiosum are typically “very small” (although they can be bigger on those with weakened immunity) as well as “shiny, and smooth” in appearance. They can be “flesh-colored,” white or pink, and they are shaped like a dome with a dent in the center. While they aren’t usually associated with pain, they can itch.
The lesions will typically show up as a solitary bump or in a “patch” of at least 20, explains the source. They can appear anywhere on the body except for the palms of hands and soles of feet, it adds. While the incubation period for the virus is from 2 to 7-weeks, the physical symptoms may not show up for 6-months, adds the source.
How is it Spread?
The CDC explains that in order to contract molluscum contagiosum, there has to be “direct” contact with a contaminated source. That can include clothing and towels, as well as pool equipment and toys, it notes. While the virus is not spread to other parts of the body through the bloodstream, scratching a lesion and then touching another area of the body can spread it, it adds.
For the older population, it is often spread through intimate contact, adds the source. In fact, “Many, but not all, cases of molluscum in adults are caused by sexual contact,” it explains. In any case, once the visible lesions are gone, it cannot be transmitted to others, it adds.
How is the Infection Diagnosed?
The American Academy of Dermatology Association (AAD) says that seeing a dermatologist for this issue can be beneficial. A qualified dermatologist can tell the difference between molluscum and another skin issue to help guide any required treatment, it adds.
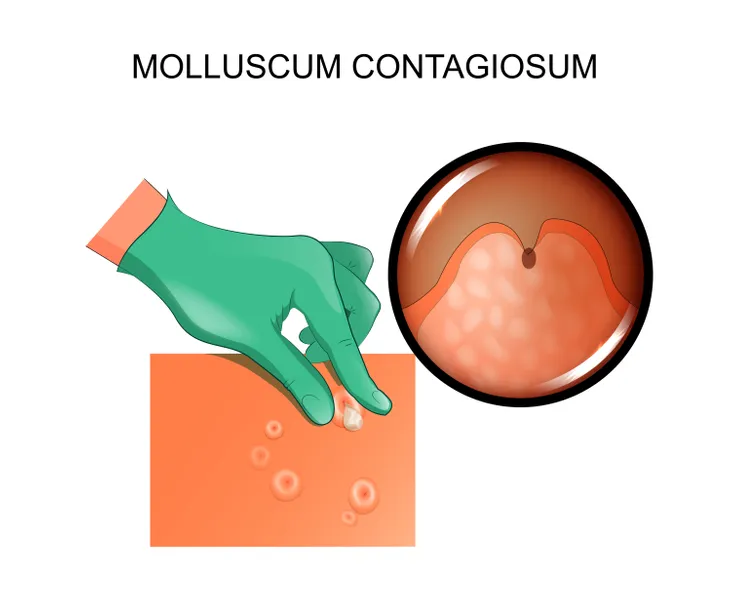
Typically, a skin expert can identify the infection by simply looking at the skin lesions, it explains. There could be some cases where they take a small sample to look at under a microscope to be sure, the source notes. If it is molluscum contagiosum, the medical professional may or may not recommend treatment depending on factors that we’ll explain next.
How Is the Infection Treated?
The AAD says that if the patient has an otherwise healthy immune system, oftentimes a dermatologist will recommend letting it clear on its own. However, treatment may be an option for those with other conditions such as eczema, bumps in the genital region, or an “extremely bothersome molluscum.”
There are a number of treatments available, such as cantharidin (also known as beetlejuice) that is applied by a professional to each bump. This causes blistering, and the bumps will clear as the skin clears, it adds. Other treatments mentioned by the source include cryotherapy (basically freezing the bumps), which can be uncomfortable for kids. It may take more than one session of these approaches to be effective.
Other Popular Treatments for Molluscum
The AAD mentions other treatment options, including pulsed dye laser (PDL) that is sometimes an option for “difficult-to-treat” cases or those with AIDS. It cites a study that suggests this treatment can be done within 2-minutes, and that the vast majority of study subjects were lesion-free within a month of the treatment.
Other routes lean more towards surgery. Curettage involves using a medical device (curette) to physically cut away the bumps, which is not painful when done with skilled hands – but it may be inappropriate for younger kids as it can seem scary. Another option is a dermatologist uses forceps or a scalpel to drain the “cheesy substance” that contains the virus inside the core of the bumps. This requires medication to numb the skin first. Do not try this at home, it warns.
There are Medications Available
Aside from cantharidin (Cantharone) treatment that is applied by a health professional, Healthline says that your doctor may decide to prescribe medications to help treat your molluscum infection. These medications include trichloroacetic acid, a topical cream called Condylox, or imiquimod (Aldara).
It warns that those who are pregnant or breastfeeding should let their doctor know before taking these medications. For those with HIV, the source says antiretroviral therapy may be the route chosen as it helps to strengthen the immune system enough to fight off infections.
Can it Be Avoided?
Medical News Today explains that taking certain measures can “help” prevent the spread of this virus. They include the standard hand washing routines, especially if there’s a case in close proximity. The source notes you can cover the infected areas to reduce risk to others through skin contact.
The site also explains that if you’re infected with molluscum, you should avoid contact sports, and older patients shouldn’t try to scratch or shave over the infected area as it can cause spread. Don’t share any of your personal hygiene items, it adds, noting any sexual contact should be avoided until all signs are gone, as a condom is not adequate skin protection.
When Will it Be Gone?
Having a molluscum infection does not mean you will have it for life. Healthline explains the lesions will often go away on their own within 6 to 12-months in people with healthy immune systems, and there won’t be scarring.
However, in some cases it can take a few years for the symptoms to disappear, it adds, and typically lasts longer in those who have immune system problems. (You can also talk to your doctor about the treatment options). Unlike some other pox like chicken pox, you can get molluscum more than once, it adds.