A blood clot can be very, very dangerous. This lump-like collection of blood platelets and plasma proteins doesn’t have to be large — often, it’s too small to even see — but by forming in a sensitive area, such as the location around the heart or in major veins leading to critical organs, can be deadly.
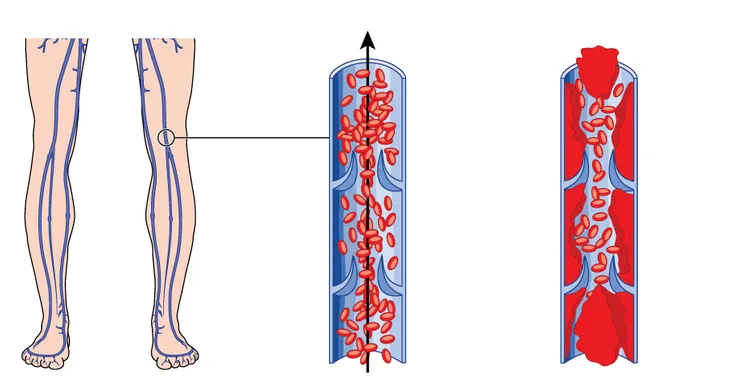
Blood clots tend to take formation in the veins in a process known as deep vein thrombosis. They’re most often formed in the legs but are also known to emerge in the heart, lungs, brain, and pelvic area. Often, blood clots are formed by lack of activity — possibly due to sitting at a desk for extremely long periods of time or undergoing surgery and being confined to a bed — physical trauma to the body, or obesity.
To get better informed on the topic, we’ve compiled a list of what to know about blood clots including the signs and symptoms, what the major risk factors are, as well as how to prevent and treat them. Take a look…
1. Defining a Blood Clot
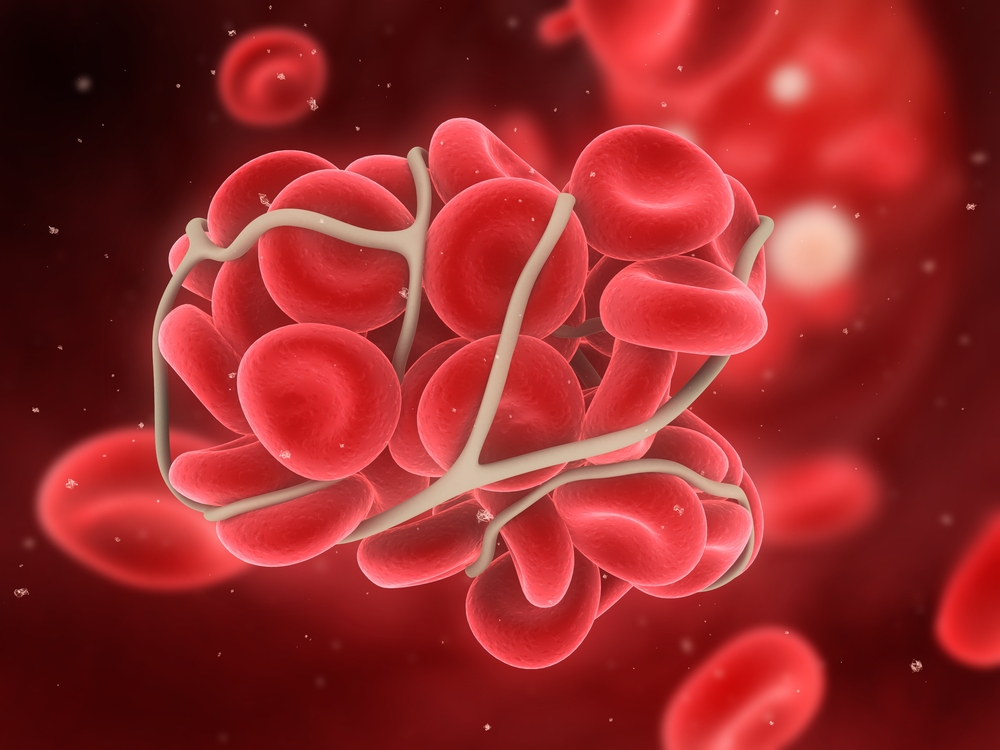
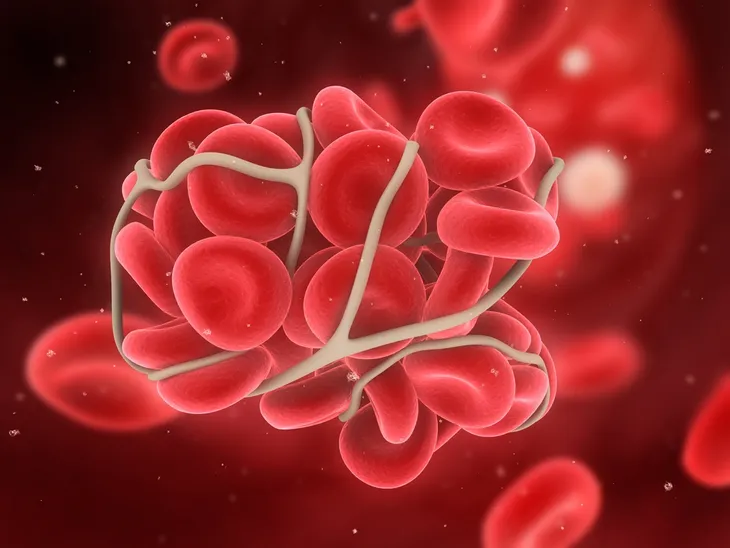
Before you can combat against blood clots, it helps to understand exactly what they are. While blood clots are healthy when they’re stopping the blood flow from a cut or injury, they can also form when they’re not actually needed, which can be a real problem, notes WebMD.
Platelets in your blood are activated by damage to a blood vessel, “changing shape to form a plug that fills in the broken part to stop blood from leaking out,” notes the source. Chemicals from the platelets further the clotting process by attracting other platelets, and then proteins in your blood (called clotting factors) end up as long strands of fibrin that get “tangled up with the platelets in the plug to create a net that traps even more platelets and cells,” it adds. While there are usually other proteins to break down the clot, but cholesterol buildup (plaques) can trigger a clot as well when they break open, it explains.
2. More Than One Type of Clot
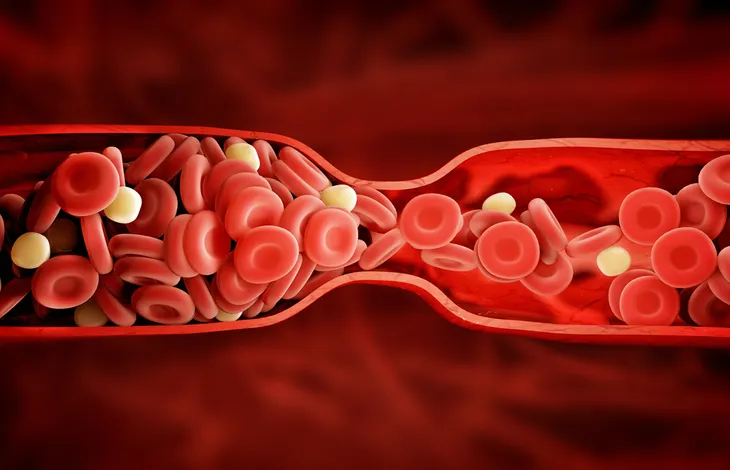
There are different types of blood clots depending on where they occur in your system, adds WebMD. While different areas of your body can be affected by clots, there are generally 2-types – arterial and venous, adds the source.
It explains that arterial clots block blood (and oxygen) from reaching vital organs, which can lead to tissue damage. They may also form in the heart or brain, setting off a heart attack or stroke. Meanwhile, venous clots in veins “tend to develop slowly,” therefore the symptoms may not be as obvious. There are different types of clots in the venous category – superficial venous thrombosis (near the surface), deep vein thrombosis (DVT), and pulmonary embolism (PE), it adds. We’ll look more at those next.
3. Going Deeper About Thrombosis
The Mayo Clinic explains that DVT occurs in a “deep vein” in your body, most often in the legs. This can set off some telltale signs in the legs, or you might not suspect anything at all, it adds.
DVT can also occur if you have certain medical conditions affecting the clotting of your blood, adds the clinic. “It can also happen if you don’t move for a long time, such as after surgery or an accident, or when you’re confined to bed,” it adds.
Signs and Symptoms
4. Redness
A slight discoloration of the skin in the area of the clot is often one of the first signs of the formation of a thrombus (or clot) deep in a vein. The cause of the skin discoloration is pretty straightforward: dense collections of blood beneath the surface of the skin become visible as they grow in size.
If you experience persistent patches of red skin in the legs, particularly after an injury or surgery, you should bring them to the attention of your doctor. The hallmark of deep vein thrombosis skin redness is that it does not go away over time, or intensifies for no immediately detectable reason.
5. Swelling
Likewise, painful swelling may occur at the site of the clot—particular if it develops in the leg, ankle, or calf area. These areas of the body have increased bone and tissue densities, making it more difficult for the body to naturally clear a clot which is already forming.
One of the telltale signs that swelling may be clot-related is that it will not respond to usual treatments, such as the application of hot or cold compresses. The swelling may also intensify for no immediately apparent reason, and may occur without external injury to the affected area.
6. Warm Skin
Blood clotting will often cause a temperature change. In leg clots, it the skin near the area may increase in temperature and become warm to the touch. Sometimes, this warm skin also presents as a persistent feeling of heat or tingling in the affected area, which is typically highly localized.
Warm skin is frequently accompanied by other symptoms, including itchiness and throbbing. Like other symptoms, these presentations typically don’t respond well to home remedies and will intensify over time if they are left untreated.
7. Fainting
Fainting and dizzy spells may occur if the body is unable to dissolve the blood clot naturally, on its own or if it detaches and travels towards the lungs. In this case, breathing may become labored. Dizziness may be most pronounced if you stand up suddenly after sitting or laying down, and because of the nonspecific nature of this symptom, many people don’t associate it with the possibility of a blood clot.
Losing consciousness is a serious symptom which should be investigated by a doctor. It also carries the risk of causing serious injury, as you could hit your head or another sensitive part of your body when you faint. Seek immediate medical attention if you pass out.
8. Increased Heart Rate
As the leg clot grows in size, the body will attempt to eradicate it and the vital organs, like the heart, will work and pump harder, resulting in an accelerated heartbeat. Abnormalities in heart function can also signal that the blood clot has left your leg and traveled to other parts of the body. If so, you’re likely to experience other symptoms, including sharp, stabbing chest pains which intensify with deep breathing.
Increases in your heart rate can also cause psychological symptoms, including anxiety and, in severe cases, panic attacks. If left unchecked, a persistently rapid heart rate can also cause a whole host of other medical problems, so be sure to get checked by a doctor if you detect these symptoms.
9. Fatigue
Any illness, such as a blood clot, will have the body’s defense systems working overtime, which may result in fatigue or exhaustion. As with many other symptoms of deep vein thrombosis, fatigue can be nonspecific, and its root cause can be difficult to diagnose. Thus, it’s important to be on the lookout for other blood clot symptoms if you’re frequently feeling tired.
The hallmark of blood clot-related fatigue is that you will feel tired for no immediately apparent reason. In other words, you’ll find yourself feeling exhausted even if you haven’t engaged in intense physical activity, and fatigue can occur even if you’re sleeping as much or more than you normally do.
10. Fever
A blood clot, particularly if it detaches and enters the bloodstream, may cause a mild or low grade fever. In addition to elevated body temperature, the symptoms of fever include sweating or shivering, a persistent headache, body weakness, dehydration, and diminished appetite.
In severe cases, fevers can cause additional symptoms, including irritability and mood disturbances, confusion, convulsions or even hallucinations. These symptoms usually occur if the body’s core temperature settles in a very high range, between 103 and 106 degrees Fahrenheit (39.4 and 41.1 degrees Celsius).
11. Tenderness
Oftentimes the skin surrounding the clot, even though it’s deep within the leg, may become quite tender to the touch with no evidence of bruising on the skin surface. The veins below the skin in the affected area may also become visible through the skin, though this typically does not occur until the blood clot reaches a relatively large size.
Note that tenderness may occur in both legs, even if only one is affected by the blood clot. This may be because you’re subconsciously favoring your stronger leg, which in turn can trigger muscle and joint strains that subsequently manifest through pain and tenderness.
12. No Symptoms
Approximately half of those experiencing a blood clot in the leg (or deep vein thrombosis) have little or no symptoms at all. While an asymptomatic blood clot is usually a sign that the thrombosis has not yet reached a serious stage, this isn’t always the case. Even large blood clots that require immediate medical attention can sometimes cause no symptoms at all until the clot dislodges and travels through the bloodstream.
This is one of the reasons it’s important to actively prevent blood clots if you’re at elevated risk. Wear comfortable, loose-fitting clothing, avoid standing or sitting for periods exceeding one hour, lower your salt intake, and remain physically active.
13. Distended Veins
Sometimes, a particularly stubborn blood clot will show itself via distention or in surface veins in or around the area of the leg where it’s developing. You should pay particular attention to this symptom if you aren’t experiencing similar phenomena in other parts of your body.
In most cases, distended veins will not result in complications or problems in and of themselves. However, in cases where a blood clot is putting significant pressure on surrounding blood vessels, internal ruptures may occur and intensified redness or bruising may result.
14. Foot Pain
Deep vein thrombosis may also cause a person to experience pain in one or both of their feet. Because this symptom doesn’t occur in the leg—the location of the blood clot—they may not make the connection and dismiss it as being caused by something else.
But the reason foot pain occurs is because the blood clot in the leg is restricting or blocking blood flow to the area. As a result, the tissues in the feet aren’t receiving enough oxygen from the blood, which causes pain.
15. Calf Pain
Having a blood clot in the leg may also cause you to experience pain in your calves. Unfortunately, however, this pain “…can easily be mistaken for a muscle cramp or strain, which is why the issue often goes undiagnosed and is specifically dangerous,” says Luis Navarro, MD, in speaking with Prevention.com.
The source indicates pain from deep vein thrombosis tends to be most noticeable when you’re walking, or when bending or flexing the foot upward. If you find yourself experiencing these symptoms, especially along with others mentioned on this list, be sure to see a physician immediately.
16. Skin Discoloration
As mentioned earlier, the hallmark symptom of deep vein thrombosis is persistent redness in the area of the blood clot. But that’s not the only skin discoloration that can occur with this condition. As a result of the blood clot, the extremities—like the ankle or foot—may become pale due to decreased blood flow to the area, in addition to feeling noticeably cooler when touched.
If the blood clot goes untreated, the area may take on a bluish tinge and feel even cooler to the touch, which Livestrong.com says “indicates that blood flow from a blood clot in the leg has become worse.”
17. Unexplained Cough
In some cases, especially for those who are asymptomatic, it may be hard to detect deep vein thrombosis until the blood clot detaches from the leg and travels to the lungs, causing a pulmonary embolism. A pulmonary embolism can be incredibly dangerous—sometimes fatal—so it’s important to recognize the symptoms.
One such symptom is a persistent, but unexplained cough (as in, it’s not being caused by an infection or other condition). For most, the cough tends to be dry, but some people may cough up mucus or blood.
18. Chest Pain and Shortness of Breath
As touched on briefly earlier, a pulmonary embolism may also cause you to experience chest pain. It may feel as though you are having a heart attack, but with a pulmonary embolism, Prevention.com says the pain “tends to be sharp and stabbing, and feels worse when you take a deep breath,” and is exacerbated by each inhalation.
In addition to chest pain, a pulmonary embolism often causes shortness of breath. For some, it may come on suddenly, regardless of whether they’ve been active or at rest, while for others it may build gradually over time.
19. Bloody Mucus with Worsening Cough
As previously mentioned, the Mayo Clinic lists a bad cough and coughing up blood as one of the symptoms of a pulmonary embolism. That is in addition to chest pain and shortness of breath.
20. Pain
The restriction in blood flow that is caused by a blood clot can also result in the affected individual experiencing a great deal of pain. This pain tends to be limited to the area where the clot is located.
For instance, if the clot is in your lungs you may experience chest pain. Or if it’s in or around your heart, you feel pain in the chest or arm. WebMD indicates that this pain generally intensifies as the clot worsens and “can range from a dull ache to intense pain.”
Risk Factors
21. Long Periods of Immobility
According to research from the American College of Phlebology, one of the most ideal environments for the formation of a deep vein thrombosis is a long stretch of sitting or immobility where muscles don’t contract.
Think about the times you sat for long periods without moving—such as on a long airplane trip, bus ride, or car trip. This immobility can drastically decrease blood flow and lead to blood clot formation. Long periods of stasis (i.e., following a surgery or injury) are also considered risky for DVT formation.
22. Age and Body Weight
Being overweight can contribute to numerous health issues, including the formation of a blood clot. Health experts at the Mayo Clinic point out that carrying around excess body weight increases the pressure in the veins in your pelvis and legs.
The Clinic also notes that individuals over the age of 60-years old are at greater risk of DVT. However, blood clots and DVT can form at age, particularly if a number of risk factors are present.
23. Pregnancy
When we’re pregnant we’re suddenly carrying around a lot of extra weight—particularly in the final trimester. The American Pregnancy Association notes that this excess pressure can increase the stress and compression on the veins in an expecting woman’s pelvis and legs.
In addition, the risk of developing a DVT or blood clot can last up to 6-weeks after a woman gives birth. This is especially true for mom’s who are inactive after birth (i.e., if they’re recovering from a caesarian).
24. Injuries or Surgeries
The folks at the Mayo Clinic find that prolonged bed rest can lead to the developing of a deep vein thrombosis following an injury or surgery.
Any prolonged period of inactivity—such as a hospital stay—can lead to decreased contraction of leg muscles, decreased blood circulation, and higher risk of a blood clot. Paralysis patients are also at high risk of DVT.
25. Genetic Predisposition
If you have a genetic or family history of DVP, consider yourself at risk of a blood clot. Research from the American Heart Association states that a family history of DVT and pulmonary embolism (or PE) are both prime risk factors for developing DVP.
In a 2011 study conducted by the Thrombosis and Atherosclerosis Research Institute on 45,362 patients hospitalized for DVT, a spike was found in DVT incidence rates in relation to genetic or familial clustering of this disorder.
26. Birth Control
The National Blood Clot Alliance notes that although birth control does not necessarily cause blood clots, some types of oral birth control medications can heighten a woman’s risk of DVT by approximately 40-percent.
The NBCA point out that both oral contraceptives and hormone replacement therapy (which contain estrogen and progesterone hormones) may intensify blood clotting factors—leaving women at risk of developing DVT.
27. Smoking
If you smoke, you already know that you’re not doing your health any favors. According to research from the American Thoracic Society, smoking impacts both blood circulation and the blood’s ability to clot—raising the risk of DVT.
However, deaths from DVT and pulmonary embolism are elevated in patients with Chronic Obstructive Pulmonary Disease (or COPD) due to a combination of factors—namely blood coagulation abnormalities and reduced mobility.
Prevention and Treatment
28. Anise Oil
Anise is a plant that produces a brilliant flower and, when harvested, its flesh has a very tart taste. It’s used sparingly by chefs who can find and afford it. Beyond its culinary purposes, it’s also popular for its medicinal uses, including helping fight inflammation, prevent infections, and relax muscles. It can even help improve blood flow and reduce pain associated with blood clots.
To use anise oil for medicinal purposes, add two or three drops to a glass of water and then drink the mixture down. You can also rub some of the anise oil into the area affected by a blood clot; this is most effective if the blood clot is visible and near the surface of the skin, such as in the legs. Repeat either application two or three times in a 24-hour period.
29. Helichrysum Oil
Helichrysum is a herb that boasts a variety of medicinal properties, including the ability to fight inflammation and limit the activity of free radicals. It’s also considered a natural blood thinner capable of reducing coagulation, which makes it a real asset for anyone trying to prevent the formation of blood clots or remove those clots after they’ve formed in the body.
Helichrysum oil doesn’t need to be ingested; instead, experts recommend you mix six or so drops of it with another type of oil, such as coconut or olive oil, and then rub it into the skin surrounding the area affected by the blood clot. You can do this up to three times daily and check each day to see the progress.
Helichrysum oil is derived from the medicinal herb, helichrysum. It has many health benefits and is known for its antioxidant and anti-inflammatory properties. It is also a natural blood thinner due to its anticoagulant properties. Thus, helichrysum oil is one of the best options to treat the blood clot in your leg.
30. Turmeric
Turmeric has been used for centuries in some of India’s most flavorful dishes. This yellow spice has a stunning appearance, striking flavor, and even more potent health benefits. For one, it contains the property curcumin, which can help prevent coagulation and, in doing so, reduce the risk of developing blood clots.
You can add turmeric to your cooking — it’s similar to curry powder in flavor — or you can add a single teaspoon to some warm milk and consume it that way. Do this once or twice a day to get the full benefit.
31. Epsom Salt
Epsom salt is known for its ability to help with a variety of ailments by using it in a bath. Supporters of doing this with epsom salt argue it can help relax the body and ease mental stress; relieve muscle pain and cramps; eliminate toxins from the body; even improve the functionality of the nerves. Most relevant to this list, epsom salt, when added to a bath, is said to improve circulation of the blood and reduce inflammation, making it perfect in helping to fight blood clots. In short, believers in epsom salt baths believe these can make one feel better both physically and mentally.
Unlike many of the other items on this list, you won’t be ingesting epsom salt but instead, adding it to your bath water. Once you’ve done that, lay down and let the saltwater mixture soak into your body for roughly half an hour. Repeat each day.
32. Garlic
Garlic may be one of the most versatile types of food available — while it may not be advisable to eat it raw, shaving raw garlic and adding it to sauces, stews and marinades can do a lot for the flavor of your favorite dishes. As for its internal properties, garlic has considerable health benefits, as it contains both allicin and ajoene, both of which can assist in treating blood clots.
You can try consuming more garlic in your food or you can prepare an odd-tasting but effective solution consisting of garlic cloves, hot water, and honey. This tea, if you can call it that, should be boiled and then consumed once it’s cooled off. If you’re looking for help with an existing blood clot, try drinking the mixture a few times each day.
33. Green Tea
Green tea has a variety of uses and, depending on who you ask, offers a range of health benefits when consumed on a regular basis. Supporters of green tea argue that its antioxidant properties can help prevent blood clots before they form, while its anti-thrombotic characteristics allow it to help thin blood clots should they emerge. At the very least, it’s a fine alternative to coffee and soda.
Today, finding green tea is very easy; it’s available at most grocery stores and pharmacies. But if you want to maximize its potential, you may want to try using green tea extract, which can be added to a cup of water and consumed with honey (for flavor). Repeat two or three times a day.
34. Oregano
Oregano, whether dried or fresh, makes an excellent addition to a variety of dishes, from roast chicken and fish to pasta sauce. But there’s more to oregano than its flavor: it also boasts a number of health-building properties, like its ability to fight free radicals and inflammation. It may even help limit the formation of blood clots.
You can add oregano to your food in order to benefit from its many health properties or you can take an oregano supplement that provides all you need for the day in a single pill. Oregano oil is also an option; simply add a teaspoon to a glass of water and take three or four times a day.
35. Vitamin E
Vitamin E boasts a collection of vitamins, known as tocopherols and tocotrienols that, together can help fight free radicals and help the body resist coagulation of the blood, making it an ideal partner in the war against dangerous blood clots.
You can take a vitamin E supplement to get the vitamins benefits, or you can simply work to get more of this vitamin in your food. Some popular foods that include a substantial amount of vitamin E include almonds, spinach, sweet potatoes, avocado, sunflower seeds, palm oil, and butternut squash.
36. Cayenne
Cayenne pepper makes an excellent addition to any meal that needs some serious spicing up. Just a pinch can transform a bland dish into something far more exotic and interesting (just be sure to avoid overdoing it, especially if you’re preparing a meal for someone who struggles with spice). But there’s more to cayenne pepper than its spicy touch: it also contains salicylates which have been shown to help thin the blood, assisting in treating and prevent blood clots.
You can either add more cayenne pepper to your food or consider taking cayenne pepper capsules, which you can take twice each day.
37. Ginger
Ginger, which is somehow both spicy and sweet, makes a useful addition to all kinds of savory and sweet dishes. But like cayenne pepper, another entry on this list, it boasts the health benefits of a compound known as salicylate, a well-known blood thinner. That makes it very helpful in either trying to prevent the formation of blood clots or helping to remove them from the body.
You can add more ginger (shaved or powdered) to your cooking or you can put together a quick drink that helps you quickly activate many of its benefits. To do the latter, peel some ginger or add the powdered variety to some hot water with honey. Once the water has cooled, drink it down and repeat a couple times each day.
38. Wintergreen Oil
You’ve probably enjoyed wintergreen-flavored mints or gum, but have you ever heard of its blood thinning capabilities? Inside the oil of wintergreen, you can find a compound known as methyl salicylate, which is the part of wintergreen with blood-thinning properties; it can also help in the fight against inflammation. For both reasons, wintergreen oil is a useful tool in helping fight blood clots.
To get the most out of your wintergreen oil, add five or six drops to another type of oil, like 30 mililitres of coconut or olive oil. Then take the completed mixture and rub it deep into the area of the body affected by the blood clot. Repeat this process one more time, making two applications each day.
39. Water
When in doubt, drink lots of water. Surprisingly, perhaps, staying hydrated can make a big difference when you’re worried about developing blood clots, as their chances of forming increase when an individual is dehydrated.
The amount of water you need each day will likely vary based on your level of physical activity, height, and weight. It may also depend on any other health issues you may be dealing with. For the average individual, between six and eight glasses of water each day should do fine, but check with your family doctor just to be sure.