- While calcium is essential for several reasons, including strong bones and teeth, too much of it can cause hypercalcemia.
- Hypercalcemia occurs when you have high blood calcium levels. Causes can include high doses of certain supplements and cancer.
- Blood tests and imaging tests can help doctors diagnose hypercalcemia and determine a treatment plan.
You probably know calcium is important for strong bones and teeth. Plus, it’s “essential for the normal function of organs, cells, muscles, and nerves,” according to Healthline. However, consuming too much calcium can lead to health problems.
For instance, high levels of calcium can cause hypercalcemia. Let’s take a closer look at the condition to help you recognize the symptoms and understand the causes. We’ll also cover treatments and preventative measures.
What Is Hypercalcemia?
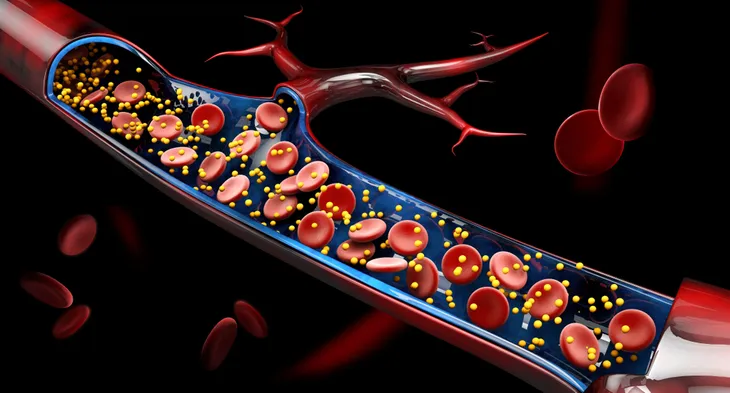
Hypercalcemia is a condition that occurs when you have too much calcium in your blood. While calcium is an essential mineral, too much calcium “makes it hard for the body to carry out its normal functions,” according to Healthline. In fact, the source says severe cases can be life-threatening.
According to the Mayo Clinic, hypercalcemia is often caused by overactive parathyroid glands. And the source says symptoms can “range from nonexistent to severe.” But we’ll get more into the details next.
Common Symptoms of Hypercalcemia
If you have a mild case of hypercalcemia, then you might not have symptoms. However, the Mayo Clinic says more severe cases can have symptoms related to the kidneys, digestive system, bones, muscles, and brain. The source says those parts of the body are affected by high blood calcium levels.
According to the Cleveland Clinic, specific signs and symptoms can include:
- Frequent urination
- Excessive thirst
- Bone pain
- Muscle aches
- Vomiting
- Constipation
- Fatigue
- Forgetfulness
Additionally, the Mayo Clinic says hypercalcemia can interfere with heart function, though it’s rare. In those cases, symptoms can include palpitations and fainting.
What Causes Hypercalcemia?
According to WebMD, overactive parathyroid glands are the most common cause of hypercalcemia. If blood calcium levels get low, then those glands release parathyroid hormone (PTH). But when those glands are overactive, they emit more PTH than your body needs. Overactive parathyroid glands are also known as hyperparathyroidism.
High doses of supplements and antacids are another cause, according to Healthline. For example, excessive use of Vitamin D supplements or antacids that contain calcium can cause high blood calcium levels. Additionally, the source says some lung diseases and cancers like tuberculosis and lung cancer can lead to hypercalcemia.
Hyperparathyroidism 101
Let’s take a closer look at hyperparathyroidism since it’s the most common cause of hypercalcemia. As previously mentioned, hyperparathyroidism occurs when you have overactive parathyroid glands. Those glands are located in your neck behind the thyroid, according to Verywell Health.
Overactive parathyroid glands release too much PTH, which “signals your body to make more calcium available,” according to the Cleveland Clinic. Your body, in turn, responds by releasing calcium from your bones and retaining calcium in your kidneys. It can lead to weak bones and kidney stones.
Less Common Causes
According to WebMD, inactivity and severe dehydration are less common causes of hypercalcemia. If you don’t put your body weight on your bones, then the source says your bones release calcium. So, those who are paralyzed or bedridden for a significant length of time can be at risk of developing hypercalcemia.
The source says severe dehydration can also lead to hypercalcemia because “your kidneys can’t get rid of calcium if you don’t have enough fluid in your body.” When you’re dehydrated, urine tends to be dark yellow instead of light yellow. If your urine stays dark after you hydrate, then talk to your doctor about severe dehydration.
Complications of Hypercalcemia
Untreated hypercalcemia can lead to several complications. According to the Mayo Clinic, complications include:
- Osteoporosis
- Kidney stones
- Kidney failure
- Nervous system problems
- Abnormal heart rhythm
Since hypercalcemia can cause your bones to release calcium and your kidneys to retain calcium, it makes sense that hypercalcemia can cause osteoporosis and kidney issues. The source says osteoporosis can lead to bone fractures and spinal curvature, while kidney failure can limit the ability of your kidneys to cleanse the blood and eliminate fluid.
Additionally, severe hypercalcemia can affect your nervous system and heart rhythm. As a result, it can lead to confusion, dementia, coma, and arrhythmia.
When to See a Doctor
If you develop common symptoms of hypercalcemia, then you should contact your doctor. For instance, reach out to your doctor if you’re excessively thirsty or urinating frequently. Before your doctor’s appointment, take some time to jot down all of your symptoms and when they started.
Also, write down every medication, supplement, and vitamin you take. Plus, make note of the dose for each one. Your doctor may ask about your medical history and stressors. So, it can help to think about those things as part of your preparation. You want to provide your doctor with as much information as possible.
Diagnosing Hypercalcemia
Hypercalcemia doesn’t always cause symptoms, so the Mayo Clinic says you might not even know you have it “until routine blood tests reveal a high level of blood calcium.” However, it may be diagnosed sooner if you’re experiencing symptoms.
In addition to discussing your symptoms, medical history, and calcium intake, your doctor will likely conduct a physical exam. According to the source, your doctor may order blood tests as well as imaging tests of your bones or lungs. Additionally, your general practitioner may refer you to an endocrinologist.
Hypercalcemia Treatments
Treatment depends on the severity of your condition and what’s causing it. If you have a mild case of hypercalcemia, then the Mayo Clinic says your doctor may take a “watch and wait” approach. In other words, your doctor may put a hold on treatment and instead monitor your bones and kidneys.
According to the Cleveland Clinic, your doctor may recommend drinking more water, cutting back on calcium-containing supplements, and switching to a non-thiazide blood pressure medicine. If your hypercalcemia is caused by hyperparathyroidism, then the source says your doctor may prescribe medication or recommend surgery.
Foods to Avoid
According to Livestrong, your doctor may recommend a low-calcium diet as part of your treatment plan. If your doctor recommends cutting back on calcium in your diet, then you may be told to avoid:
- Dairy products: Milk, cheese, ice cream, yogurt, etc.
- Calcium-fortified products: Certain cereals, orange juices, etc.
- Seafood products: Salmon, sardines, shrimp, crab, etc.
- Certain vegetables: Spinach, kale, broccoli, etc.
However, the source says you shouldn’t self-treat with a low-calcium diet. Instead, you should seek doctor supervision.
Hypercalcemia Prevention
While hypercalcemia can’t always be prevented, you can take certain steps to lower your risk. For example, the Cleveland Clinic recommends “avoiding excess intake of calcium pills and calcium-based antacid tablets.” Before taking vitamins and supplements, always talk with your doctor to get the correct dose.
Additionally, Healthline emphasizes the importance of drinking enough water. The Mayo Clinic says eight glasses of water a day is a reasonable goal, but everyone has unique needs. So, you may need more or less. Fortunately, the source says, “Most healthy people can stay hydrated by drinking water and other fluids whenever they feel thirsty.”
What Is the Outlook?
The outlook for people with hypercalcemia depends on the cause and severity. According to the Palliative Care Network of Wisconsin, cancer-related hypercalcemia often has a poor prognosis. The source says approximately 50-percent of patients will pass away within 30-days of diagnosis, “which suggests that hypercalcemia is a sign of hormonally advanced cancer.”
But if a different reason causes your hypercalcemia and your blood calcium levels are slightly high, then the Cleveland Clinic says you’ll likely have “few or no health complications.” Of course, you should talk with your doctor about your specific case. And be sure to follow your treatment plan and attend follow-up appointments.