Iron is an essential mineral that the body needs for growth and development. It helps produce hormones and makes hemoglobin, which is a vital protein our red blood cells need to carry oxygen from the lungs to all parts of the body. But is it possible to have too much iron in your body?
As it turns out, the answer is yes, and this condition is known as hemochromatosis. Leaving hemochromatosis untreated can cause serious damage to the body, which is why early intervention is so important. To better understand this disorder, let’s take a look at the common symptoms and causes of hemochromatosis, as well as how to diagnose and treat it.
What Is Hemochromatosis?
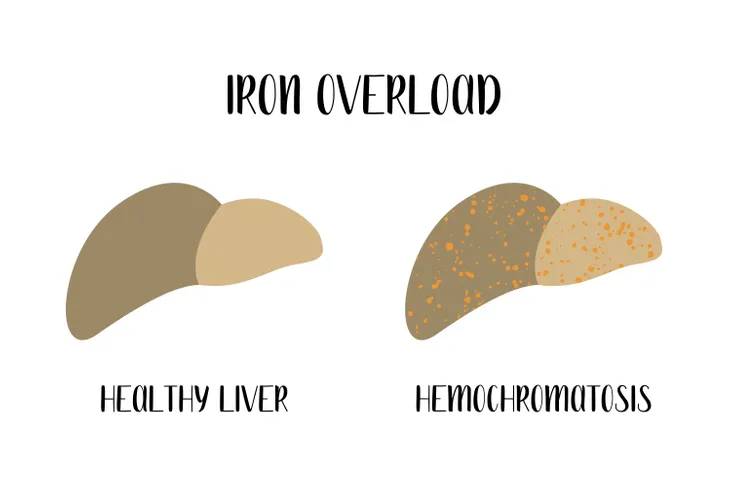
In short, hemochromatosis is a disorder where too much iron builds up in your body. There are two types of hemochromatosis: primary and secondary, which we’ll get into more detail later.
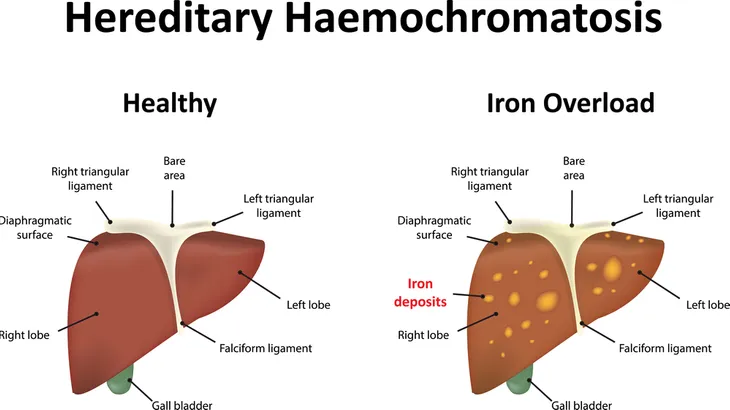
Hemochromatosis can be a serious health problem because your body can’t eliminate excess iron. Iron can build up in important organs, such as the liver, heart, pancreas, pituitary gland, skin, and even in your joints. If this happens, it can cause organ and tissue damage.
Symptoms of Hemochromatosis
Unfortunately, hemochromatosis doesn’t always present noticeable symptoms, and in some cases, it is only diagnosed after a blood test or normal screening.
However, if an individual does have symptoms, they may include fatigue, weakness, weight loss, abdominal pain, low libido, a bronze or gray skin color, and joint pain. It’s worth noting, if symptoms do arise, they can vary from person to person.
Causes of Primary Hemochromatosis
As we mentioned earlier, there are two types of hemochromatosis, with the first being primary hemochromatosis (also referred to as hereditary hemochromatosis). This type is caused by genetic factors that control how much iron an individual absorbs from food.
Healthline explains, “Usually, a person with hereditary hemochromatosis inherits a copy of the defective gene from each parent.” Although it’s worth mentioning, not everyone who inherits the gene will develop the disorder.
Causes of Secondary Hemochromatosis
The second type of hemochromatosis is secondary hemochromatosis which occurs from another medical condition (such as erythropoietin hemochromatosis). This is a disease in which red blood cells release too much iron into the body. This happens because the blood cells are too fragile.
There are several risk factors for secondary hemochromatosis, including alcohol dependency, taking iron or vitamin C supplements, or frequent blood transfusions. A family history of liver disease, heart disease, or diabetes can also increase your risk.
Risk Factors
Some risk factors may increase your chances of having this disorder. As mentioned earlier, genetics play a factor. Medical News Today says, “Having two copies of a faulty HFE gene is the main risk factor for hereditary hemochromatosis.” This means you inherit one copy of the gene from each parent.
Certain ethnicities may have a higher risk of developing hemochromatosis. This includes Caucasian individuals of Northern European descent. Medical News Today also notes that this disorder is less common in individuals of African American, Hispanic, Asian, and American Indian descent.
Do Gender and Age Play a Role?
Men and women are both at risk for developing hemochromatosis, however, it may affect females less. This is because females lose blood during menstruation, which in turn, reduces iron levels. However, once a woman enters menopause, they may develop symptoms because iron levels can build up.
Furthermore, men who have this medical condition, don’t typically develop symptoms until they are 40- to 60-years old.
How Is Hemochromatosis Diagnosed?
If you are experiencing symptoms of hemochromatosis or suspect you may have a build-up of excess iron, make sure you talk with your doctor. Diagnosing this condition can be a little tricky because other conditions can have similar symptoms.
To diagnose this condition your doctor will first ask a variety of questions regarding your symptoms, supplement intake, and family history. Along with a physical exam, your doctor may also request a blood test, genetic test, magnetic resonance imaging (MRI), or a biopsy. Let’s look more closely at what these entail next.
Blood Testing
Two types of blood tests can help determine high levels of iron, including a transferrin saturation (TS) test, and a serum ferritin test. A TS test displays how much iron is bound to transferrin, which is a protein that carries iron in your blood.
In contrast, a serum ferritin test measures the amount of ferritin, which is a protein that stores iron in your blood.
Genetic Testing
Your doctor may also request genetic testing to determine if you have hemochromatosis. A DNA test can confirm whether or not you carry the gene that may lead to this disorder.
If you suspect you have a family history of hemochromatosis, your doctor may draw blood, or use a swab to collect cells from your mouth to get test results.
Biopsy and MRI Tests
Lastly, your doctor may also require a MRI or a liver biopsy to determine if you have high levels of iron. An MRI scan is less invasive than a biopsy and can also measure the iron levels in your body.
If your doctor requires a biopsy, they’ll remove a small piece of tissue from your liver and test it in the lab. The liver stores most of the iron in your body and is typically one of the first organs to be damaged by hemochromatosis.
Treating Hemochromatosis
Early detection is essential if you want to prevent organ damage. However, if organ damage has already occurred, then treatment may be able to help prevent more damage.
When hemochromatosis is left untreated, it can lead to severe organ damage, and in some severe cases, it can even be fatal. Let’s take a look at the treatment options for hemochromatosis.
Phlebotomy
The most common medical treatment for hemochromatosis is phlebotomy. This procedure involves a needle and tube that takes blood and iron from the body.
Typically, 1-pint of blood is removed once or twice a week for the first part of treatment. Once your iron levels return to normal, you may only need the treatment every 2- to 4-months.
Chelation
Another treatment option is chelation, which helps your body expel the extra iron. Your doctor may inject the drugs or prescribe pills.
Keep in mind this treatment option may have side effects, such as pain at the injection site or flu-like symptoms. It can also be expensive and may not be suitable for individuals with heart complications.
Dietary Changes
Finally, making some dietary changes can help reduce your iron intake, and in turn, may help reduce symptoms of hemochromatosis. First, if your iron levels are normal or high, avoid taking supplements that contain iron. You should also avoid taking vitamin C supplements because this vitamin increases iron absorption.
Another dietary change you can make is limiting your alcohol consumption because alcohol can damage your liver and reduce your intake of iron-rich foods. If you do have hemochromatosis, your doctor will be able to determine the best treatment option for you.
The Risks of Leaving Hemochromatosis Untreated
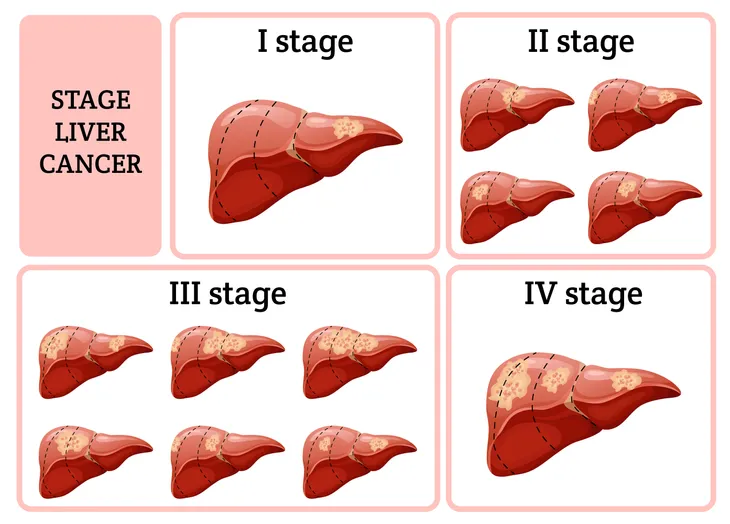
Leaving hemochromatosis untreated can have serious consequences and lead to health complications, such as cirrhosis. It may even increase your risk of liver cancer.
Other health complications include diabetes, congestive heart failure, irregular heart rhythms, arthritis, osteoporosis, depression, gallbladder disease, and some other types of cancer. As you can see it’s imperative that you receive treatment if you have hemochromatosis. To ensure your levels are within a healthy range, book an appointment with your doctor.