Parkinson’s disease is a debilitating, progressive nervous system condition that can happen to anyone. Sufferers can experience tremors, slow movement, slurred speech, difficulty eating, and a slew of other symptoms. According to the Parkinson’s Foundation, there are 60,000 people diagnosed each year in the United States and 10 million people living with the disease throughout the world.
Parkinson’s progresses and presents differently for each individual which tends to create some myths and misconceptions. Because of this, we’ve created a list of the most common myths and found the real facts behind them. Take a look and learn the truth about Parkinson’s disease….
1. Parkinson’s Disease Only Happens To Older People
When most people hear Parkinson’s disease, they tend to associate this disease with older people. While that is true for the majority of people with Parkinson’s disease, it’s very possible to be diagnosed as a young person. If someone is diagnosed before the age of 50 they will receive a Young Onset Parkinson’s Disease (YOPD) diagnosis. According to the Parkinson’s Foundation, “YOPD affects about two to 10-percent of the one million people with PD in the United States.” A very rare condition called juvenile Parkinsonism can happen in children and teenagers says the Parkinson’s Foundation. This form of Parkinson’s disease is typically connected to genetic changes.
The symptoms of YOPD are similar to the ones older people experience. However, younger people can have very different challenges because of their diagnosis. Raising a family, job, and other social issues can make their experience different and unique from an older person. It’s important to have a support system in place if you have Parkinson’s disease or offer support to friends and family if they have been diagnosed. It’s a lifelong condition that will affect every aspect of their lives.
2. There Is No Treatment
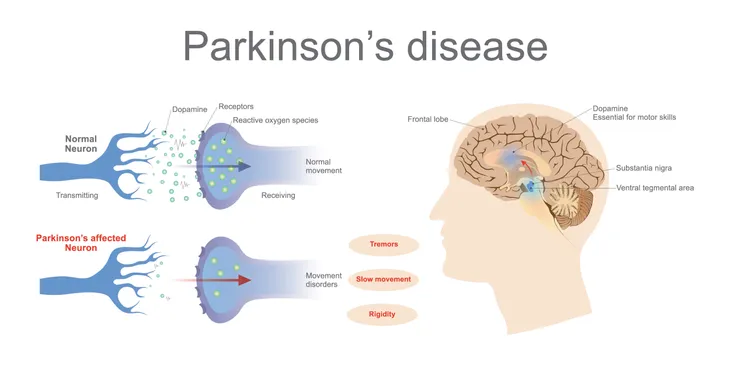
Thankfully this myth couldn’t be further from the truth. There are multiple medication options out there that treat the symptoms of Parkinson’s disease. One of the most common medications is carbidopa-levodopa. It helps to increase the dopamine levels within your brain, lessening the motor symptoms of Parkinson’s.
Other common treatments used to help control symptoms are physical therapy, deep brain stimulation, massage, Tai Chi, yoga, and meditation according to the Mayo Clinic. Determining which combination of treatment is best for you will depend on the severity of your disease progression and symptoms. Talk to your doctors to decide your best options.
3. Parkinson’s Disease Is A Genetic Disease
Unfortunately, there is no known definitive cause for Parkinson’s disease. The Parkinson’s Foundation tells us that, “researchers believe there are both genetic and external factors that lead to the development of PD, but there is not a single definitive genetic mutation that leads to all cases of PD.” When we see people suffer from terrible diseases we want to place blame, point our finger at something that is causing the pain. Researchers are working to find that one thing to blame but haven’t found it yet.
We know that Parkinson’s disease can run in some families, but approximately 90-percent of diagnoses are in people without a family history, reports the Parkinson’s Foundation. If you have a family history of Parkinson’s disease, let your doctor know and learn as much as you can about the signs and symptoms of the disease. Early diagnosis and treatment can improve your quality of life.
4. Everyone Experiences The Same Symptoms
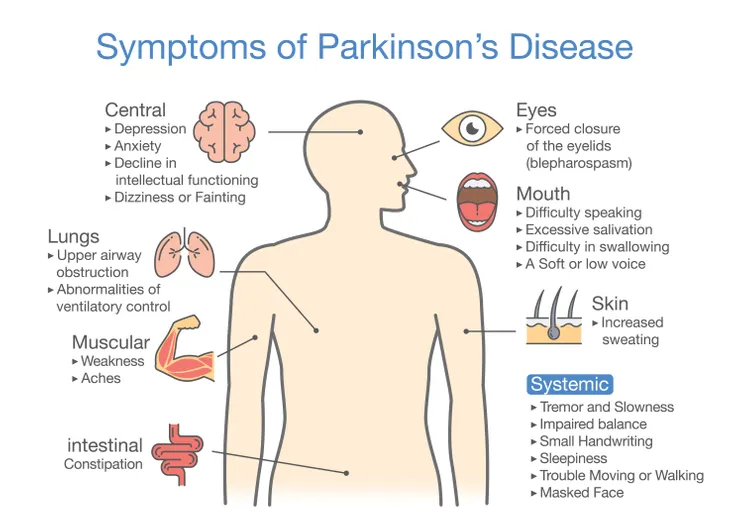
One common myth is that everyone with Parkinson’s disease will have the same symptoms and experiences. Yet, like with every disease and condition, each person experiences symptoms differently. The Michael J. Fox Foundation for Parkinson’s Disease tells us that, “for some people, tremor is the first symptom they experience, while others never see tremor or don’t for many years.”
Symptom severity and disease progression vary from person to person. Some people will have symptoms like slow movement and rigid muscles while others will not. If you have been diagnosed, your doctor should give you a sense of possible symptoms and how they can be best treated.
5. It Only Involves Physical Symptoms
It’s easy to see the outward signs of Parkinson’s disease. It’s the emotional and non-motor symptoms that aren’t visible to outsiders that can also take a significant toll on a person’s body. People with Parkinson’s disease can experience dementia, anxiety, depression, sleep problems and so much more according to John Hopkins.
If you are experiencing non-physical symptoms due to your Parkinson’s disease keep a record for your doctor. Many of these symptoms can be treated. Now more than ever, doctors are aware of the emotional impact of Parkinson’s disease and want to help improve their patient’s emotional and physical well-being.
6. Parkinson’s Disease Can Flare Up
Another myth is that Parkinson’s disease can have occasional flare-ups or exacerbations. But the Parkinson’s Foundation tells us that this is just not true. Parkinson’s disease is a slowly progressing condition that changes over time. People can have bad days, but major changes should be investigated by a doctor.
Anyone with Parkinson’s disease that has a change in health or behavior should see their doctor. Numerous causes can make Parkinson’s disease symptoms worse. According to the Parkinson’s Foundation, some causes are infections, dehydration, medications, and urinary tract infections. You should talk to your neurologist to evaluate a specific cause to an abrupt health change.
7. Medication Will Stop Working After A Few Years
The belief that a common medication used to treat Parkinson’s disease, levodopa, will stop working after five years is untrue according to the Parkinson’s Foundation. This misconception is so widely held that some patients have refused to start levodopa or delay their doses in fear that it will stop working.
In truth, levodopa doesn’t treat every symptom of Parkinson’s disease. The medication can reduce some of the motor symptoms and can improve your quality of life. Your doctor is your best resource in determining which treatments are right for your symptoms in your stage of disease progression.
8. Medication Is The Only Treatment
Thankfully medication is not the only treatment for Parkinson’s disease. It is a helpful treatment and can lessen the symptoms of the disease but it’s not the only option. A study reported by John Hopkins found that those with Parkinson’s disease who exercised for one hour once per week were able to do more physically. Exercise also helps to improve strength and flexibility.
Another treatment is deep brain stimulation (DBS). John Hopkins says that it “is a procedure in which doctors place electrodes in the brain at the point when medications are less effective in masking motor symptoms, such as tremor, stiffness, and slowness of movement.” This treatment has been used for 20 years and “…works very similarly to a pacemaker, except the wire is in the brain, not in the heart.”
9. Parkinson’s Disease Is Predictable
Chronic diseases like Parkinson’s disease follow a different path for each person. Symptoms start at different stages and progress at their own pace. You may think you’re on one trajectory but then something will change and you’ll take a completely different path.
The only predictable thing about Parkinson’s is that it’s unpredictable. No one can definitively say who will be diagnosed or exactly how your life will change. But you can take control and work with your doctors to manage the symptoms of this disease. Look into support groups or talk to other people with Parkinson’s disease to help cope with your diagnosis.
10. Everyone With Parkinson’s Disease Has Tremors
Tremors are one of the most identifiable Parkinson’s disease symptoms but not everyone with the disease will experience a tremor. The progression and clinical symptoms of Parkinson’s disease are unique to every individual. “Tremors can also be caused by other conditions, including stroke, multiple sclerosis, or traumatic brain injury,” according to Parkinsonsdisease.net.
A side effect of some Parkinson’s medications is dyskinesia, another term for involuntary movements. This may initially look like a tremor but is a different movement. Dyskinesia can happen if your dose is too high. Let your doctors know if this is happening and they will adjust your medication timing or dose.
11. All Symptoms Are Related To Parkinson’s Disease
Don’t let a Parkinson’s disease diagnosis take the blame for all of your symptoms. Numerous symptoms should never be connected to Parkinson’s disease like chest pain, shortness of breath, fever, headache, and loss of muscle strength says Parkinson’s Disease Foundation. It can be life-threatening to ignore these symptoms and believe they are just another manifestation of Parkinson’s disease.
Since Parkinson’s disease is a slowly progressing condition any symptom that is new or comes on suddenly needs to be talked about with your doctor. It can be an indication of an infection or a new condition.
12. There’s No Hope with Parkinson’s Disease
Finding out that you or a loved one has Parkinson’s disease can be devastating. With no known cure and slow progression, it is both painful to watch and experience. But there is so much hope and progress happening within the research field. Researchers are working to find more effective treatments and even stop Parkinson’s from occurring.
It’s so important to work as a team with your doctors, therapists, and family when you have Parkinson’s. The impact of the disease can be overwhelming to even the most prepared people. If you are having a hard time managing the stress of medications, appointments, and symptoms let your doctors know. They can help guide you through this scary time and show you the right path.