- Colon polyps are formations of cancerous or noncancerous cells on the lining of your colon or rectum.
- Once diagnosed, colon polyps can be removed.
- Specific lifestyle choices help lower the risk of polyps reappearing.
- Colon polyps shouldn’t be ignored, as even noncancerous formations can eventually develop into colon cancer, which can be fatal.
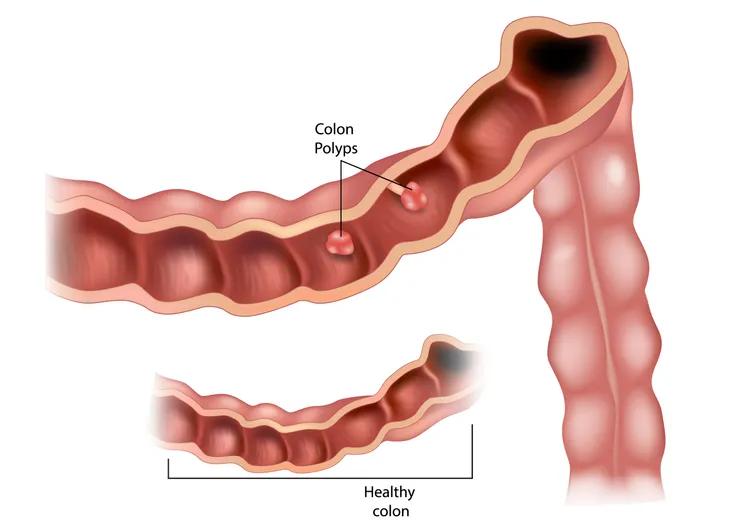
A colon polyp is a small growth of cells on the inner lining of the colon or rectum. Not all colon polyps are cancerous, but some may be. A polyp can take on different shapes, being flat, raised, or raised on a stalk.
Luckily, colon polyps aren’t something you have to live with forever. Once diagnosed, you can have your colon polyps removed, and lifestyle changes can help ensure the condition doesn’t reappear. Here’s a look at what you need to know about colon polyps.
What Are Colon Polyps?
Colon polyps are cells that grow on the lining of your large intestine or rectum. Polyps can take on a variety of shapes and be flat, raised (sessile), or formed on a stalk (pedunculated).
Many colon polyps cases are harmless. However, even if a polyp starts off as noncancerous, it can grow larger over time and develop into cancer. If colon cancer is found in its later stages, it can be fatal.
If you suspect you have a colon polyp, speak to a doctor immediately. They can determine if a polyp is present and if it’s cancerous, providing treatment if necessary. If the polyp isn’t cancerous, they can monitor the area to ensure it doesn’t develop into colon cancer over time.
What Are the Symptoms of Colon Polyps?
When colon polyps are in their early, harmless stage, they often don’t cause any noticeable symptoms. That’s why regular colon screening is so important.
Still, sometimes there are signs. Possible symptoms of colon polyps are:
- Bleeding from the rectum, either visibly seen by the naked eye or detected with a fecal blood test.
- Sudden and unexplainable iron deficiency to the point of anemia.
- Drastic and inexplicable weight loss.
- Changes in a person’s typical bowel movement patterns, such as constipation or diarrhea that lasts more than a week.
- Abdominal pain.
- Changes in stool color.
How Common Are Colon Polyps?
In the United States, colon polyps are quite common, and it’s estimated that one in four adults age 50 or older have them.
Approximately 70-percent of all colon polyps are adenomatous (also known as adenomas), meaning noncancerous. As a result, adenomatous polyps aren’t typically overly concerning. Even if they become dangerous, they usually take several years to turn cancerous. Regular colonoscopies and screenings can help catch this common type of colon polyp early before it turns harmful.
Causes of Colon Polyps
It’s perfectly normal for cells to grow and divide. However, some gene mutations can cause cells to continue to grow and divide, even when more cells aren’t needed. When this happens in the colon or rectum, the cell growth can create polyps.
Polyps can develop in anyone, but certain factors put an individual more at risk. Knowing what these risks are and making appropriate lifestyle changes is especially important for those who’ve had colon polyps in the past.
Who’s at Risk of Getting Colon Polyps
Men and women from all ethnic backgrounds are equally at risk for getting colon polyps. However, it has been found that the risk is slightly higher for Black Americans.
Generally speaking, anyone can get colon polyps. Still, there are some risk factors that increase the likelihood of developing colon polyps:
- Being over the age of 50
- Having close family history (parent or sibling) with a history of colon polyps or cancer
- Excessive smoking or alcohol consumption
- Obesity
- Inadequate physical activity
- Diabetes
- A high-fat diet
Hereditary Disorders and Risk of Colon Polyps
While rare, a handful of hereditary disorders can cause colon polyps to form. These genetic disorders include:
- Gardner’s syndrome
- Familial adenomatous polyposis Lynch syndrome (hereditary nonpolyposis colorectal cancer)
- MUTYH-associated polyposis
- Peutz-Jeghers syndrome
- Serrated polyposis syndrome
If you have any of these conditions, you should be extra vigilant about going for regular screenings and colonoscopies. These hereditary polyp disorders significantly increase a person’s risk of developing colon cancer. Early detection can be life-saving in this situation.
Diagnosing Colon Polyps
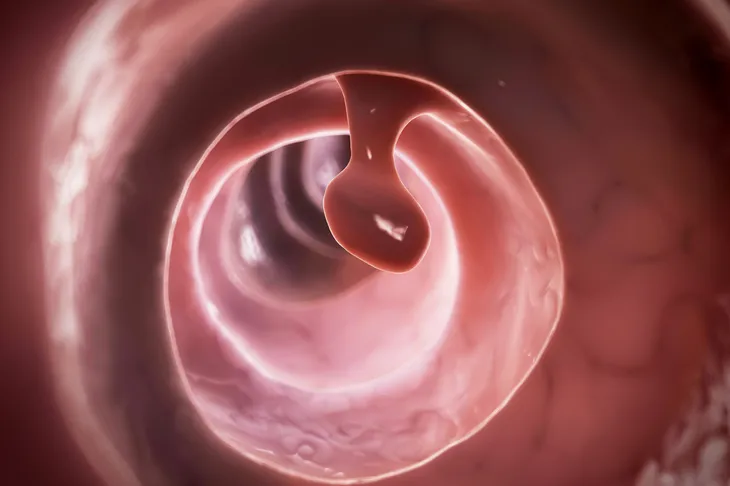
There are a few tests your doctor may order to confirm a diagnosis of colon polyps. Stool samples can be tested for the presence of blood or genetic mutations that indicate the potential formation of polyps. If the stool test comes back positive, a colonoscopy is the next step. In this procedure, a thin, flexible tube is inserted into the rectum. The tube has a camera attached, which can capture images of any polyps present.
A sigmoidoscopy may also be performed, during which a thin, flexible tube is inserted into the rectum to examine the sigmoid colon (the part of the large intestine closest to the colon). A sigmoidoscopy is less invasive than a colonoscopy. Some physicians may opt for a CT scan, which uses radiation to capture an image of the large intestine.
Treatment for Colon Polyps
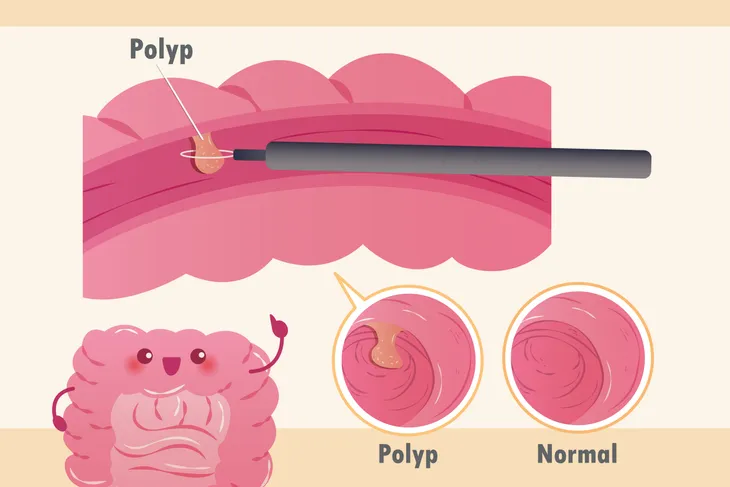
Doctors can often remove polyps during the bowel examination. Forceps are used to remove the polyps in a procedure called a polypectomy. Sometimes, a liquid needs to be injected underneath the polyp to lift it from the surrounding tissue before removal. If a polypectomy is unsuccessful, minimally invasive surgery may be required instead.
After removal, the cells are sent to a lab for a biopsy to test the tissue. If the cells are determined to be cancerous, you may need to receive cancer treatment.
After removing the polyps, your doctor will tell you how often you should be screened. Your screening frequency depends on the number and size of your polyps, the microscopic analysis of the cells, and any risk factors you may have.
Risks of Polyp Removal
Colon polyps removal is a relatively straightforward procedure. Still, as is the case with any medical procedure, some risks are involved. One of the risks of polyps removal is bleeding at the polypectomy site. The bleeding can start during the procedure or several days later. If bleeding persists for several days, contact your doctor. Another colonoscopy may be needed to stop the bleeding.
The other risk is perforation (a hole or a tear) of the colon. Perforations from polyp removal are uncommon. If this happens, the gap can sometimes be closed with clips during another colonoscopy. Otherwise, minor surgery may be necessary.
Prevention
As mentioned, everyone is at risk for colon polyps. But you can take some steps to reduce your chances of developing this condition:
- Eat a healthy diet that’s low in fatty foods
- Get regular exercise at least three times a week
- Maintain a healthy weight
- Quit smoking
- Avoid drinking excessive amounts of alcohol
- Eat less meat
- Eat more fiber and calcium-rich foods
Regular screenings can’t prevent colon polyps from developing, but they can detect polyps early so that they can be removed before becoming cancerous.
 Shutterstock/wavebreakmedia
Shutterstock/wavebreakmediaFollow-Up Care
If your doctor has diagnosed you with colon polyps and treated you for them, know that removal isn’t the end of the treatment. Having colon polyps puts you at an increased risk of having them again and of developing colon cancer.
Your doctor will likely recommend you return for a colonoscopy. The frequency of your checkups might be:
- In 5-10 years, if you had one or two polyps.
- In 3-5 years, if you had three or four polyps.
- In 3 years, if you had five to 10 polyps, polyps bigger than 10 millimeters, or specific higher-risk types of polyps.
- Within 6-months if you had more than 10 polyps, a huge polyp or a polyp that had to be removed in pieces.
When to See a Doctor
If you suspect you have colon polyps, speak to a doctor right away. Colon polyps don’t go away without treatment and need to be removed and examined.
The good news is that, in most cases, colon polyps aren’t life-threatening. Treatment is quick and screening ensures you stay healthy and safe. A colonoscopy may not be very enjoyable, but it could potentially save your life.
If you have colon polyps, consider encouraging your immediate family members to get screened too. Genetics is a risk factor for colon polyps, so parents, siblings, and children may also have the condition.