There are a number of conditions that could lead to damage of your large bowel. Luckily, the medical world has you covered. A procedure called a colectomy can remove the diseased sections to treat certain health conditions, and put the healthy parts back together in many cases.
If you have a colectomy coming up and are feeling nervous, you can rest easy because this procedure has been around for several decades. In fact, the first mention of a right colectomy to treat cancer was in 1893. It’s also fairly routine. More than 300,000 colectomies are performed each year in the U.S. So, you can look forward to getting on with your life after some recovery. Let’s take a closer look at why a doctor would recommend a colectomy, what’s involved in the process, and what you can expect post-surgery.
Why Would I Need a Colectomy?
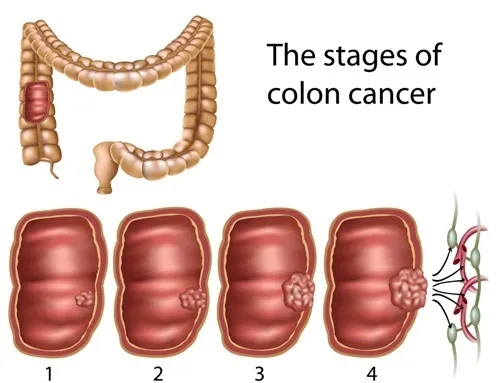
A colectomy – also known as a large bowel resection – may be the chosen approach to treat several medical conditions. For example, Healthline explains one reason why it might be done is to tackle colon cancer. Other reasons may include removing pre-cancerous polyps or clearing intestinal blockages due to tumors or scar tissue.
Several other common medical issues might be addressed by a colectomy. They include diverticulitis, volvulus (twisted bowel), ulcerative colitis, and intussusception, “which occurs when one part of your intestine slides into another part of your intestine,” explains the source.
How to Prepare for Surgery
The Cleveland Clinic explains that before your surgery, you may be instructed to drink a “special liquid” meant to empty your bowel, as well as take antibiotics to prevent infections. Fasting may also be required before the procedure.
In some cases, you may be instructed by your doctor to stop taking certain medications ahead of time, as they can potentially increase risks during the procedure. You’ll likely also be asked to bring a few days’ worth of supplies (such as toiletries and activities) for your hospital stay.
Open Surgery vs. Laparoscopic Colectomy
Surgeons may use open surgery or laparoscopic surgery. Open surgery means the surgeon will make one (or more) long incisions to access the affected colon tissues.
A laparoscopic colectomy is often preferred because it’s less invasive compared to open surgery. It involves making tiny incisions and guiding flexible tools using a video monitor. Your surgeon will be able to determine which route is best for you.
How Long Is the Surgery?
The length of the surgery will vary for every individual. That said, it can take anywhere from 1-hour or it may take longer, up to 4-hours. Ultimately, the duration of the surgery will depend on how much colon tissue your surgeon needs to remove.
What Happens During the Surgery?
The procedure will be done while you’re asleep (general anesthesia). The surgeons will carefully separate the affected bowel tissue and reconnect the healthy parts using staples or sutures.
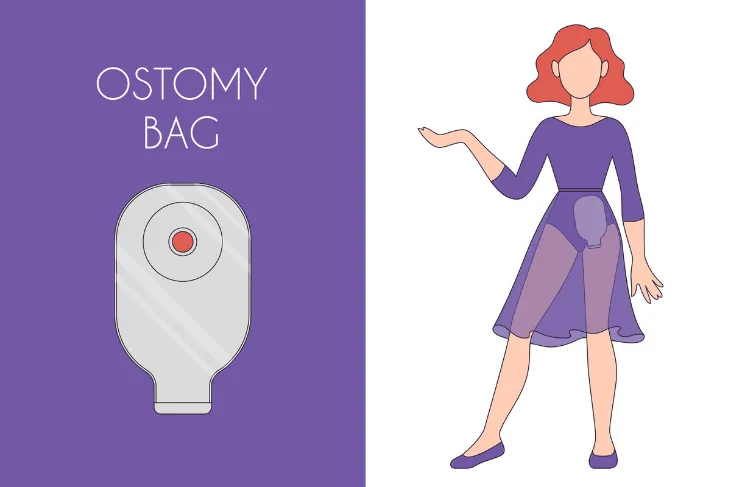
A colostomy procedure may be required as well if the healthy ends of your colon can’t be reconnected, notes the Cleveland Clinic. In this case, a small opening is made in the abdominal wall, with the healthy end of the colon attached to it. The colostomy bag is then attached.
Is a Colostomy Bag Permanent?
If you’re worried the colostomy bag will be permanent, you should know it isn’t always permanent. Some individuals only temporarily need a colostomy bag while their colon heals. If this is the case, you’ll have a second operation to reconnect the colon and remove the bag.
In some cases, the colostomy bag is permanent and is used as a waste removal solution afterward. Ask your surgeon if you’ll need one ahead of your surgery. While the thought of a permanent colostomy bag can be daunting, don’t worry. There are trained professionals at the hospital who will teach you how to care for it and how to manage life as normally as possible.
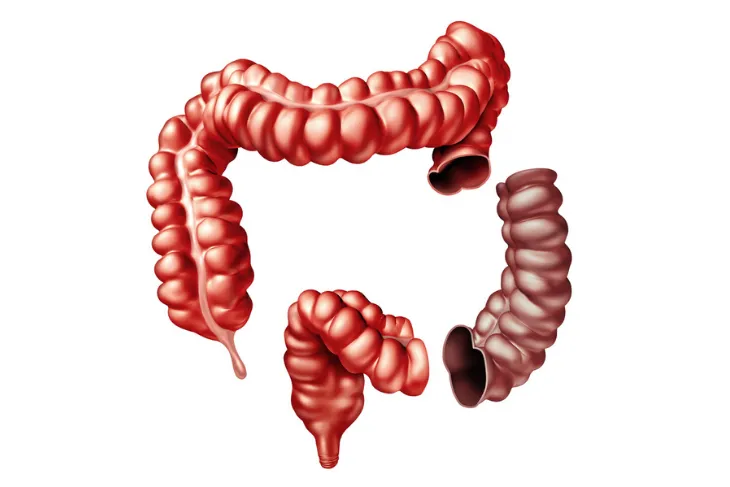
Does the Entire Colon Need to Be Removed?
The quick answer is, no. The Mayo Clinic points out there are different types of colectomy procedures for different situations. While there are times when the entire colon needs to be removed, in some other cases only a portion needs to be taken out.
A partial colectomy, also known as a subtotal colectomy, removes just a section of the colon. A hemicolectomy means removing either the right or left portion, while a proctocolectomy means discarding the colon and rectum. The type of colectomy you receive corresponds to the issue you’re dealing with, and its severity.
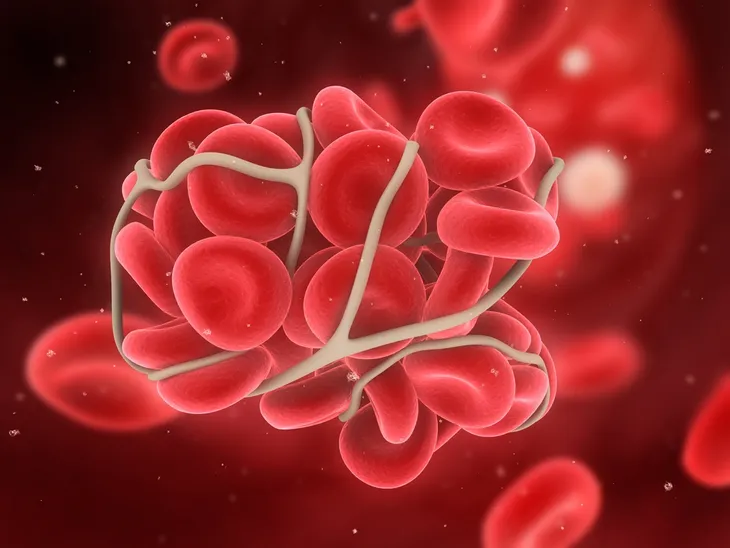
Are There Any Surgical Risks?
All surgeries carry some level of risk, as noted by Healthline. But some of the risks associated with a colectomy include infections, blood clots, difficulty breathing, and pneumonia, says the source. There’s also a chance of heart attack or stroke, it adds. In fact, major surgery not related to the heart may lead to cardiac issues within a year, according to research.
The source adds, there are some risks that are more specific to lower bowel resection. They include abdominal bleeding, an “incisional” hernia, damage to other organs (such as the bladder), and dehiscence (when a surgical wound opens up).
What Does the Initial Recovery Entail?
Verywell Health says the rate of recovery from a colectomy largely relies on the overall health of the patient before the surgery. There are other factors including the patient’s age, lifestyle (whether they smoke and get regular exercise), and diet.
You can expect to be in the hospital recovering for 3 to 7-days (on average) following the major procedure. During this time, the medical staff will look for any complications including infections or blockages from scar tissue.
What Can You Eat After a Colectomy?
While your colon is healing, you may need to modify your diet. Your doctor may recommend a low-fiber diet (such as white pasta and bread) for up to 1-month post-surgery. Cleveland Clinic says, “These foods create less work for your colon while it’s trying to heal.”
Increasing your daily water intake may also be necessary. Your doctor will likely refer you to a trained dietitian who will help you make the right diet choices after your surgery.
How to Be Comfortable at Home Post-Surgery
Verywell Health points out that there’s more to consider beyond the hospital stay. For example, it will be more difficult for the patient to get around at home after being released. With that in mind, it suggests keeping the patient on a single level, which is ideal for showering and rest.
Staying on a single level will also help when using the bathroom. Up to six bowel movements per day are expected following this kind of procedure. “It might help your loved one conserve energy if they have access to, or can rent, a bedside commode for a few weeks,” the source notes.
Other Things to Consider Post-Surgery
Make sure to stock up on important medications so they’re ready when the patient returns home. Verywell Health notes pain medications may be prescribed.
If an infection occurs at home, home care nurses may be suggested by the surgeon. But be sure to call your doctor if there’s increasing pain (that’s not helped by medication), a fever of 101-Fahrenheit or more, sudden swelling in the abdominal region (especially with nausea or vomiting), or signs of confusion and lethargy.