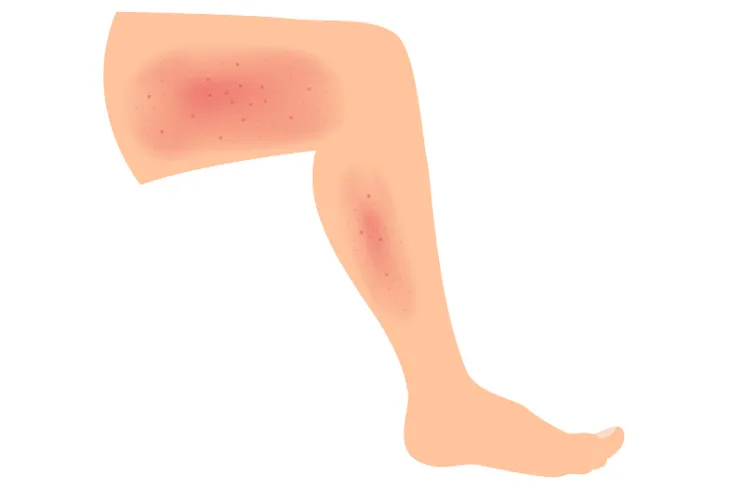
Cellulitis is one of the most commonly occurring soft tissue infections on the planet, but don’t let its ubiquity lull you in to a false sense of security. If left untreated, what starts as a patch of discolored and irritated skin can become fatal quickly. Skin affected by cellulitis will often appear red, swollen, warm, and painful to the touch. It typically appears in the legs, but can also show up in the face and arms (or any part of the body for that matter).
So, what is it, how does it happen, and what can you do to prevent it? Those are exactly the kinds of questions that this article sets out to answer for you. Let’s get started.
What Is It?
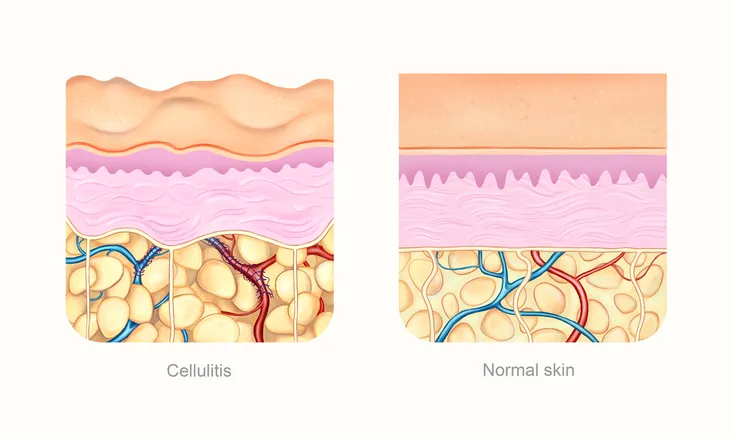
First things first, what exactly is cellulitis?
Cellulitis is a bacterial infection that occurs most frequently in middle-aged and older adults. Often associated with redness, tenderness, and warmth to the touch, cellulitis can shift and change, creating a vast array of uncomfortable and downright dangerous symptoms.
It’s also not something that will just go away in a day or two. Without proper treatment, cellulitis does have a tendency to spread to a patient’s lymph nodes and bloodstream, with life-threatening potential.
Causes
Streptococcus and staphylococcus, two widely occurring bacteria, both have the capacity to survive on many of the surfaces that we interact with on a daily basis (even on our own skin). Most of the time, these bacteria are relatively harmless and safe to cross paths with. Sometimes though, they find their way in to a patient’s skin, usually through a small cut, crack, or break in the surface of the skin, and that’s when the trouble can start.
It doesn’t matter if it’s an animal bite, a hang nail, an unbandaged paper cut, or even a patch of particularly dry skin, if it comes in to contact with one of the two bacteria mentioned above, you’re susceptible to cellulitis and all of the nasty symptoms that come along with it.
Symptoms
Cellulitis doesn’t always present itself in the same way, which is what makes seeking a professional diagnosis that much more important.
Having said that, the most common symptoms include:
- Swelling of the skin
- Tenderness to touch
- Pain
- Warmth to the touch
- Red spots
- Blisters
- Skin dimpling
- Fever
- A red and expanding area of skin
A quick internet search can provide you with a helpful visual of the symptoms, although again, cellulitis doesn’t always present itself with the same collection of symptoms every time.
One more item of note, cellulitis is a localized infection that tends to appear on one side of the body or one patch of skin.
When to See a Doctor
As we mentioned previously, cellulitis can go from an inconvenient skin irritation to a life-threatening blood infection shockingly fast. It can be treated safely and easily but only through an antibiotic and, if needed, bandaging.
If you notice swelling, tenderness or a warm rash that seems to be expanding, it’s best that you see your family physician soon as you can. If, however, you’re experiencing all of these symptoms and also have a fever, it’s important for you to seek out emergency medical care immediately.
Again, cellulitis is treatable but can be life-threatening if you’re not careful. If you notice its symptoms, know that it’s time to visit a doctor.
Treatment Options
Once a doctor has taken the necessary samples and diagnosed a case of cellulitis, they’ll often consider your age, health, and symptom severity before settling on one of the many available treatment options.
Antibiotics, wet dressings on the infected areas, surgery, rest, pain medicine, elevation of the affected limb, and topical antibiotics are most often used to ease discomfort and treat the bacterial infection.
It’s difficult to know which combination of treatments is best without the tests and experience of a licensed professional.
Risk Factors
Even the healthiest person in the world could hypothetically find themselves in a battle with cellulitis. That’s not to say that everyone is at equal risk. Predisposing conditions that increase an individual’s risk of cellulitis do exist.
Something as ordinary as an insect bite can increase your risk of cellulitis. Any disruption in the skin barrier, really. Eczema, psoriasis, and any other cause of skin inflammation are also risk factors.
Other conditions that can increase an individual’s risk of developing cellulitis include obesity, diabetes, pre-existing skin conditions, and edema (swelling).
Prevention
As previously mentioned, cellulitis can occur in anyone. No one is immune, but there are precautions that you can take to decrease your risk of encountering this painful infection.
Good personal hygiene is an essential part of keeping yourself safe from the bacteria that cause cellulitis. Wash your hands often, apply lotion on dry or cracked skin, use gloves to protect yourself from cuts and scrapes, and wear protective footwear when needed.
If you do have an open wound, ensure that it is properly bandaged and that the bandage is changed every day, or as soon as it becomes dirty or wet. It’s also important to keep your cuts and scrapes clean using an over-the-counter antibiotic ointment, such as polysporin.
The Takeaway
Cellulitis can happen anywhere, to anyone, at any time. Its severity can shift and change, and if left untreated it can become fatal.
But, it’s not all doom and gloom. The first step in preventing it from happening to you is understanding what causes it, as well as the symptoms, treatments, risk factors, and measures you can take to prevent it. Know that a proactive approach to your personal hygiene practices can dramatically decrease your risk of infection.
It’s also important to remember that cellulitis is much more than your ordinary skin rash. If you notice a patch of skin that’s sensitive or warm to the touch or if you develop a fever at the same time, seeking professional and immediate care is absolutely essential.