Strokes are a common occurrence that can change people’s lives forever. In some cases, there’s almost complete recovery, while in other cases, it can land a patient in a wheelchair indefinitely.
However, knowing more about strokes can help you identify one and take action to minimize the damaging effects or prevent a fatality. Here are 12 things we actually know about strokes, to replace what we think we know about them…
Strokes Are Not Just an “Old Person” Problem
We often think about strokes striking the elderly, but they happen at significant rates to those under the age of 65 as well. In fact, according to GoRedForWomen.org, about 25-percent of strokes occur in those under the age of 65.
There’s no minimum age for a stroke either. The source notes that they can also affect infants. They can actually be more dangerous in younger people because they are unexpected and the symptoms are more often ignored.
Stroke Symptoms Aren’t Subtle
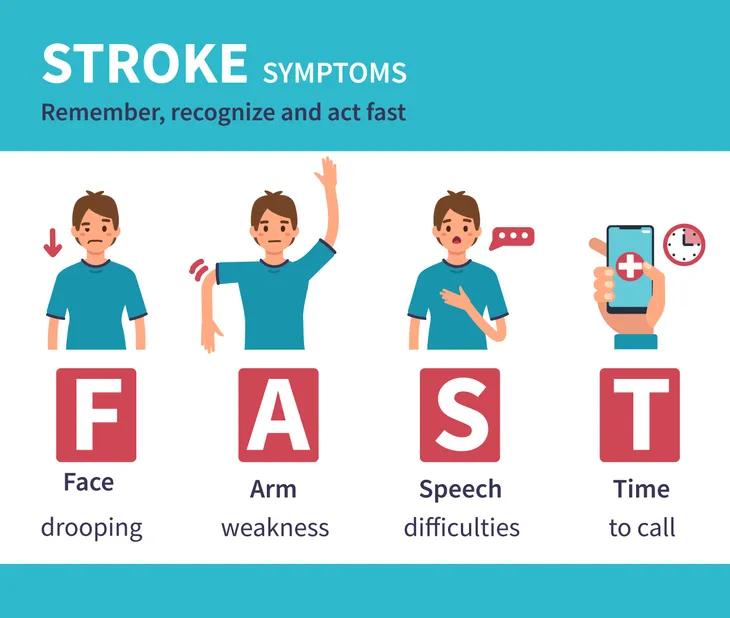
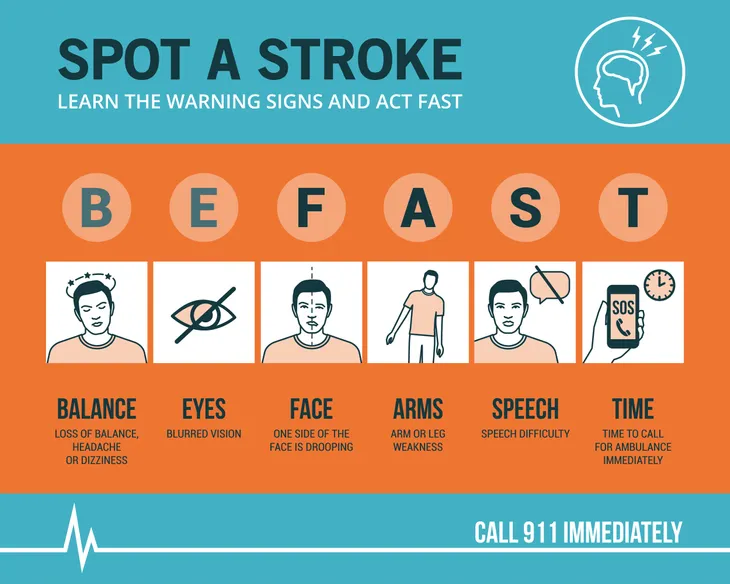
The same source says you don’t have to be a medical professional to recognize when someone is suffering a stroke. “Three-quarters of the time, even a lay-person can diagnose a stroke very easily,” notes GoRedForWomen.
The site notes you can apply the FAST test, which refers to the face, arm, speech, and time. If you see facial droop, and/or the victim is slurring their speech, those are pretty obvious signs to get medical help as quickly as possible.
Women Are Not Immune to Strokes
There seems to be a school of thought that women are more shielded from strokes than men, but statistics show women are at high risk as well. In fact, an article from Harvard Medical School explains that, while men’s stroke prevalence has decreased slightly over recent years, women’s stroke rates remain constant.
In particular, ischemic strokes, which account for about 87-percent of strokes in the U.S. and are associated with blood clots blocking blood flow to the brain, have dropped in men over the past decade, but not in women, says the source. Factors keeping stroke rates constant in women include diabetes, high blood pressure, irregular heartbeats, and pregnancy-related conditions (such as gestational diabetes and preeclampsia).
Strokes are Preventable
Again, some people accept that if a stroke happens, there isn’t anything they could’ve done to prevent it. However, the National Stroke Foundation outlines a number of health risk factors that you have control over.
For example, lifestyle factors such as eating habits and exercise levels can make a big difference in stroke risk. There are also medical factors, that can be addressed, such as high blood pressure, high cholesterol and circulation problems. There are some factors out of your control – for example, being of African American descent doubles the risk. Family history also plays a role (i.e., genetics).
Don’t Try a DIY Approach
CBS News has a few warnings about avoiding medical care in a stroke situation. One of them is not ignoring any telltale symptoms, as a doctor can use clot-busting drugs (if less than 3 to 4 1/2-hour, depending on the source) or surgery to limit the damage.
This same rule applies to mini-strokes, also known as transient ischemic attacks (TIAs), which produce similar symptoms but disappear within 24-hours. However, a patient can be at higher risk of a full-blown stroke once they’ve experienced a mini-stroke. The source also warns that you shouldn’t try to “sleep off” symptoms such as numbness or weakness, which won’t help and will waste valuable time getting medical help. Oh, and popping aspirin won’t help strokes, that’s reserved for heart attack symptoms.
Stroke Recovery is Rarely Speedy
If you’re asking how long it will take to completely recover from a stroke, you may be asking the wrong question. In some cases, symptoms can linger long after the stroke and may never fully disappear.
Stroke recovery doesn’t only happen in the first few months following the incident, says the National Stroke Association, which adds, “recovery is a lifelong process.” Of course, physical therapy and certain medications can help improve lost function and help prevent future strokes, respectively.
There are Genetic Factors
Even if you practice a healthy lifestyle and don’t smoke, you’re not immune to a stroke. You may still be at higher risk based on whether your immediate family has suffered a stroke previously, notes the Centers for Disease Control and Prevention (CDC).
Genes that have been passed down to you from your parents can contribute to stroke risk factors such as high blood pressure and even sickle cell disease (an inherited red blood cell condition more prevalent in African Americans). “People with a family history of stroke are also likely to share common environments and other potential factors that increase their risk,” adds the CDC.
A Stroke is Not a Type of Heart Attack
These are two distinct medical episodes that should be addressed and treated differently. “They may share some similarities, but they are very different medical conditions,” explains MedicalNewsToday.com.
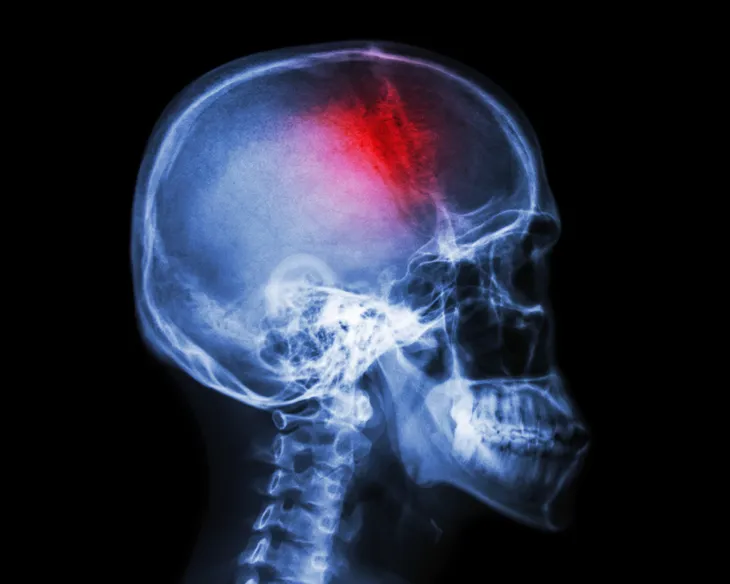
It’s about the blockage of blood flow. In a heart attack, blood flow is blocked to the heart, while in a stroke, blood flow to the brain is typically impeded. Heart attacks can cause light-headedness and dizziness, but strokes can cause weakness in the face, arm, or leg, which is usually contained to one side of the body, explains the source.
Pain is Not The Biggest Symptom of Stroke
Unlike some heart episodes, you may not feel any pain at all during a stroke. While GoRedForWomen.org lists sudden severe headaches as a possible sign of a stroke, it’s usually sudden weakness in facial muscles or a limb that tips people off as to what’s happening.
The most common telltale signs of a stroke include numbness or weakness in the face or arm/leg on one side of the body, confirms the source. It can also be accompanied by confusion and trouble communicating, blurred vision, and/or trouble walking.
Strokes are Not Rare
If you’re one of the believers that strokes only strike the unlucky few, we have some news for you. StrokeCenter.org explains that, in the U.S., stroke is actually the third leading cause of fatalities, accounting for more than 140,000 fatalities in the country each year.
Looking at the bigger picture, the source adds that almost 800,000 people suffer a stroke each year in the U.S., and these strokes are the leading cause of long-term disability. So take steps to improve your lifestyle to lower your risk, even if your family has never had an associated problem.
You’re Not in The Clear After a Stroke
Unfortunately, a stroke is not like chickenpox, as in, once you’ve had it, you won’t have it again (although chickenpox can come back later as the more sinister disease called shingles). Especially in the case of mini-strokes, you may be at higher risk for a more serious health episode, even though the stroke symptoms pass relatively quickly, says Harvard Medical School.
“Don’t be fooled by the disappearance of symptoms. Even after they are gone, danger still lurks in the form of other TIAs, stroke, and even death,” notes the source. In fact, a 2005 study shows that of all patients with TIA in the Cincinnati area, 14.6-percent suffered a full-blown stroke in the first 3-months following the initial mini-stroke.
You Probably Won’t See it Coming
While heart attacks can have telltale signs leading up to the episode in some cases, strokes can appear out of nowhere without any warning, explains GoRedForWomen.org.
“You can have a stroke with no warning signs and no symptoms, other than the stroke itself,” says the source, which is associated with the American Heart Association. In fact, it’s called a stroke because it happens so suddenly, adds the site. Don’t ignore symptoms, even if you felt great a few moments earlier.