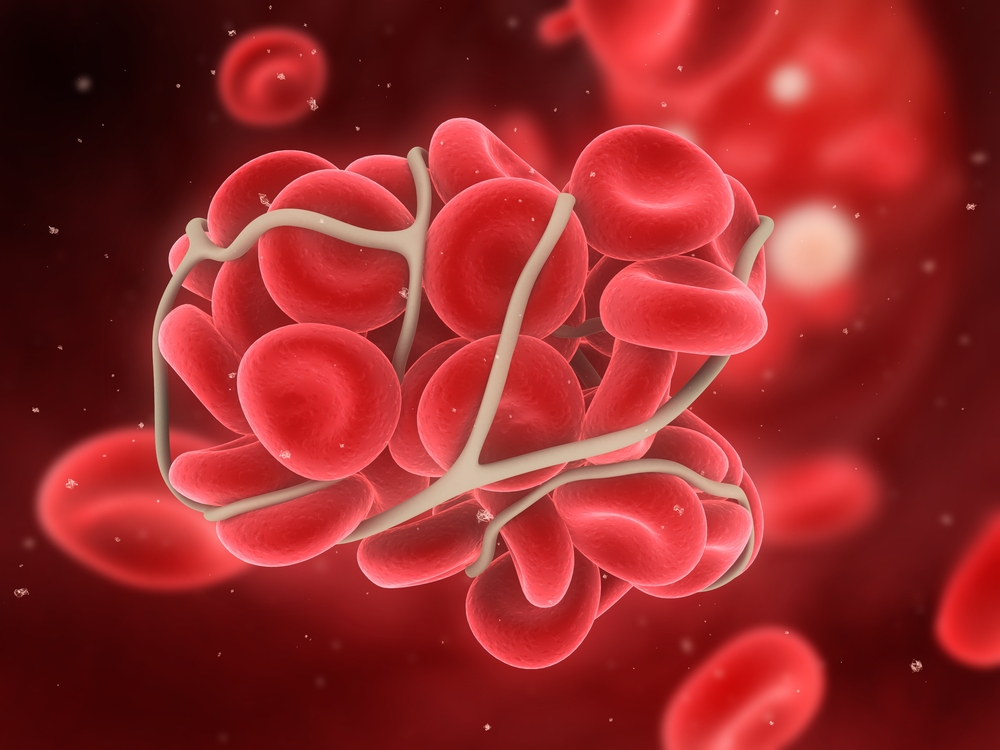
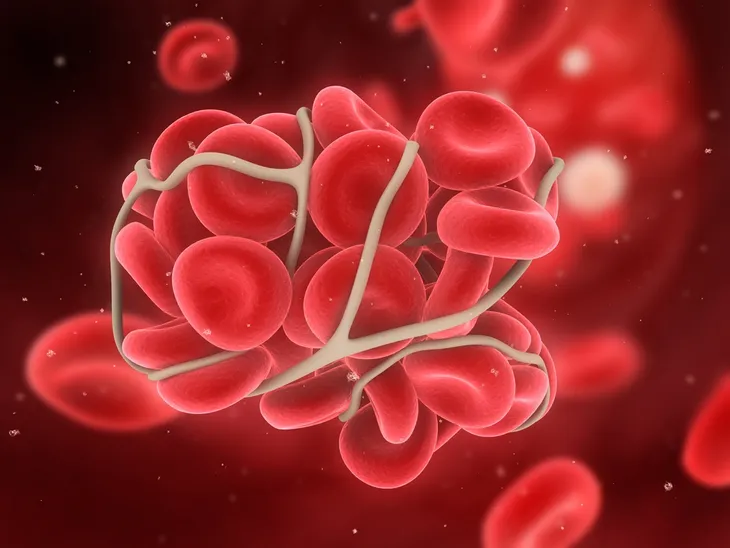
In short, a blood clot is a clump of blood that has transformed from a liquid to a semisolid. Clotting is a necessary process that we need. It helps your wounds heal and prevents you from losing too much blood. While this process isn’t dangerous on its own, it can be a threat if a blood clot forms in your veins and doesn’t dissolve on its own.
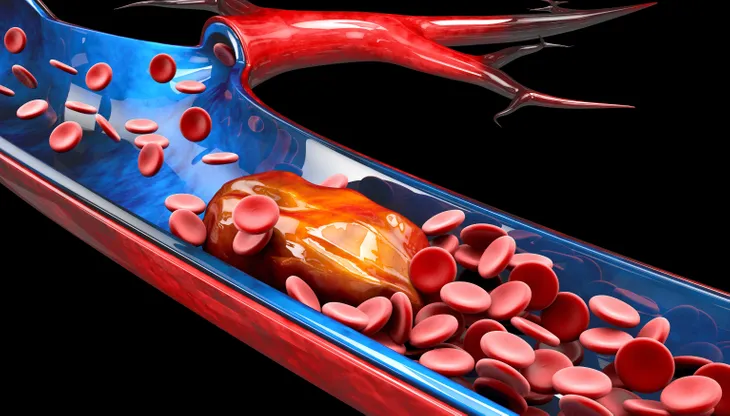
When the blood clot travels to the heart or lungs, it can get stuck and prevent blood flow. If this occurs, this is a medical emergency. To help you get informed, we’ll share everything you need to know about blood clots including the different types, the symptoms and risks, and what treatment options are available.
It’s important to note, if you think you have a blood clot, don’t wait! It can be a life-threatening situation so, call your doctor immediately.
Types of Blood Clots
There are two main types of blood clots, including a venous clot and an arterial clot. A venous clot develops in a vein and they typically build up slowly over time. They can be life-threatening, with the most serious type being deep vein thrombosis (DVT).
An arterial clot, on the other hand, develops in an artery. This type will cause symptoms right away and they also require immediate emergency attention. A telltale sign that you have an arterial clot is pain and/or paralysis in parts of the body. They can also lead to a stroke or heart attack.
Deep Vein Thrombosis (DVT)
When a clot forms “in one of the major veins deep inside your body,” this is known as deep vein thrombosis (DVT), explains Healthline. The most common place for this to occur is your legs, however, the clot can also form in your arms, pelvis, lungs, and brain.
DVT and pulmonary embolism (a venous clot that affects the lungs) affect up to 900,000 Americans each year and cause about 100,000 fatalities annually. The only way to confirm you have a blood clot is through medical guidance. And knowing the signs will help you get the medical attention you need. Let’s take a look at the common signs of a blood clot in various parts of the body.
Signs of a Blood Clot in Your Leg or Arm
The lower leg is one of the most common spots for a blood clot to develop, Akram Alashari, MD, a trauma surgeon and critical care physician at Grand Strand Regional Medical Center tells Healthline. They can also occur in the arm. If this happens typical symptoms you’ll experience include swelling, pain, a warm sensation, tenderness, and a reddish discoloration.
Symptoms will vary depending on the size of the clot. When the clot is small, individuals typically don’t develop any symptoms or they may have minor swelling and pain. However, if the clot is large you’ll likely feel a lot of pain. Healthline also points out, “It’s not common to have blood clots in both legs or arms at the same time.”
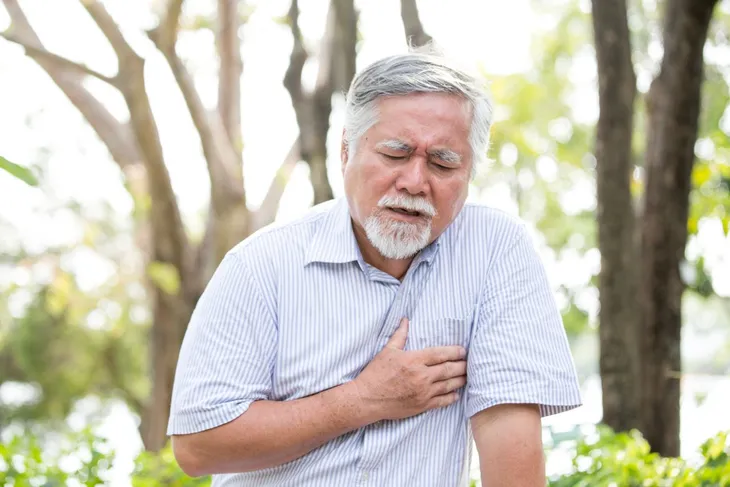
Signs of a Blood Clot in Your Heart
A blood clot in the heart may be less common than some other locations in the body but they can still happen. They’re also incredibly serious because they cause a heart attack.
Common signs of a blood clot in your heart include severe pain in your chest (that can travel down your arm), a feeling of heaviness on your chest, sweating, difficulty breathing, and lightheadedness. If you experience any of these symptoms, dial 911 right away.
Signs of a Blood Clot in Your Abdomen
WebMD explains, “blood clots can happen in the veins that drain blood from your intestines.” These are often caused by conditions such as liver disease, diverticulitis, and in some cases, even by birth control pills.
Telling signs that you have a blood clot in your abdomen includes nausea or vomiting, severe pain in your belly (which may get worse after eating), diarrhea, and bloody stools. These symptoms can also indicate other health problems such as a stomach virus or food poisoning. So, it’s best to get your symptoms examined by a doctor.
Signs of a Blood Clot In Your Lungs
WebMD points out, “a blood clot in your lung usually starts out in a deep vein in your arm or leg…” When the blood clot travels to your lungs, this is known as a pulmonary embolism (PE).
Common symptoms of a PE include sudden shortness of breath (that isn’t caused by exercising), chest pain, coughing and coughing up blood, dizziness, and heart palpitations. This is a very dangerous condition and requires medical attention right away.
Risk Factors
Certain factors can increase your chances of having a blood clot. Cleveland Clinic explains, “blood clots become more common as people get older, especially when they are over age 65.” A long hospital stay, surgery, or trauma can also greatly increase your risk.
Other less common factors include being overweight/obese, living a sedentary lifestyle, and smoking. Birth control pills, hormone replacement therapy, being pregnant, having cancer, or family history can also increase your risk.
When to See a Doctor
According to the Centers for Disease Control and Prevention (CDC), “about half of people with DVT have no symptoms at all.” This is why it’s so important to call your doctor if you suspect you may have one.
Symptoms that develop out of nowhere (such as chest pressure/pain, difficulty breathing, or shortness of breath) are even more concerning. If this occurs you should contact your local emergency services right away.
How Are Blood Clots Diagnosed?
Symptoms of a blood clot can be similar to other health conditions so, your doctor may perform a variety of tests to confirm the blood clot and to rule out other causes. If your doctor suspects you may have a blood clot, they may order a blood test.
Your doctor may also request an ultrasound to get a clear view of your blood flow and veins. A computed tomography (CT) scan may also be necessary. This imaging test can help get a clear view of the head, abdomen, or chest. Finally, magnetic resonance angiography (MRA) or V/Q scans may also be necessary to diagnose a blood clot.
What Can You Do to Prevent Its Fatal Effects?
In some cases, blood clots can be life-threatening. Luckily there are steps you can take to help prevent their fatal effects. For starters, the CDC says you should know your risks and recognize the symptoms.
At your next checkup, be sure to inform your doctor if you have any risk factors for blood clots. If you are scheduled to have surgery, talk to your doctor about blood clot risks. Finally, if you develop symptoms don’t wait and contact emergency services or your doctor right away.
Treatment: Medication and Compression Stockings
Your treatment will depend on where the blood clot is located and how likely it is to harm you, says Cleveland Clinic. One treatment option is medication. Blood thinners, also called anticoagulants, can help prevent blood clots from forming. In life-threatening situations, thrombolytics are used to help dissolve a blood clot that has already formed.
If you’re at risk for blood clots, your doctor may recommend compression stockings. These are tight-fitting stockings that provide pressure in your legs to help prevent blood clots from forming.
Treatment: Surgery
In some cases, surgery is necessary. In one procedure called catheter-directed thrombolysis, a specialist will direct a catheter (a long tube) to the blood clot. The catheter is then used to deliver medication right to the blood clot in order to help it dissolve. Thrombectomy surgery is another option in which the doctor will use special instruments to remove the blood clot.
If necessary, your doctor may need to use a stent to keep a blood vessel open. Finally, if an individual is unable to take blood thinners, “a filter is put into the inferior vena cava (the body’s largest vein) to catch blood clots before they can travel to the lungs,” says Cleveland Clinic.