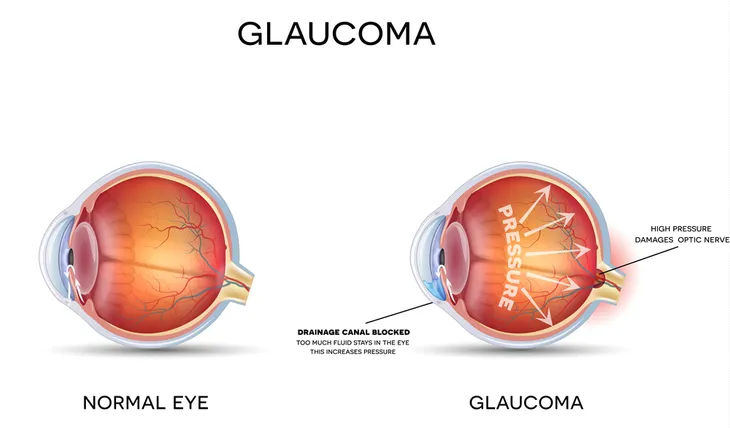
Glaucoma causes progressive and permanent vision loss due to a buildup of pressure in the eyeball. The disease presents itself in two common forms — primary open-angle glaucoma and angle-closure glaucoma. Unfortunately, both have their own unique and subtle set of symptoms, in which the unaffected eye counterbalances the vision loss in the affected eye.
Primary open-angle glaucoma, the most common type, begins in the peripheral vision and works inward to incapacitate central vision, leading to tunnel vision, while acute angle closure glaucoma (also called chronic angle-closure or narrow-angle glaucoma) causes blurred vision with halo effects. Both types cause the irreversible and gradual damage of the optic nerve (which is responsible for sending visual information from the retina to the brain). The slow decline of sight often means the condition isn’t diagnosed until an advanced stage.
You can prevent glaucoma with regular optical exams (with a visual field test) and also by remaining watching for subtle warning signs. Twelve risk factors for glaucoma are…
Advanced Age
As with many other health conditions, advanced age puts you at an increased risk for developing glaucoma, particularly if you are 60-years of age or older. Unfortunately, for some people of African-American descent, the risk increases much earlier (i.e., around the age of 40). People who fall into a high-risk age group should be getting an eye exam on a regular basis, about once a year.
Family History
We should all be up to date with our family’s medical history, especially the ones with a track record of diseases and conditions. This is because family history plays a major role in the potential risk factors for glaucoma. People who have a family history of glaucoma are at a greater risk of developing the disease by association with family members and genetics.
This means if you’re related to someone with glaucoma, you may be more susceptible to developing the condition yourself. It also means that your family line may carry the defective genes that make humans prone to glaucoma.
Ethnicity
Ethnicity is a major risk factor for glaucoma. As previously mentioned, African-Americans are more likely to develop this condition. While most people’s risk doesn’t start until the age of 60 and older, they are at a heightened risk by the age of 40.
According to The Glaucoma Foundation, other ethnicities that are at a higher risk for developing glaucoma are those of Latino ancestry and Asian descent. “People with African and Latino ancestry have a greater tendency for developing primary open-angle glaucoma than do people of other races. People of Asian descent are more prone to develop angle-closure glaucoma and normal-tension glaucoma,” writes the source.
Eye Pressure
A slightly higher internal eye pressure (or elevated intraocular pressure [IOP], which also referred to as high IOP) will also increase a person’s chances of developing glaucoma. If you know that you do have elevated IOP, regular eye exams are important. VisionAware notes that most eye care professionals “define the range of normal intraocular, or ‘within the eye’ pressure (IOP) as between 10 and 12 mm Hg [i.e., millimeters of mercury, which is a pressure measurement].” It also goes on to say that people with glaucoma often have an IOP of more than 21 mm Hg.
Existing Medications
There is some evidence that links steroid use to glaucoma. The Glaucoma Research Foundation cites a 1997 study that was published in the Journal of American Medical Association which found that glaucoma was linked to long-term corticosteroid use, particularly in long-term allergy sufferers.
The study found a 40-percent increase in “the incidence of ocular hypertension and open-angle glaucoma in adults who require approximately 14 to 35 puffs of steroid inhaler to control asthma,” writes the source. This includes eye drops, pills, inhalers, and creams, says VisionAware. Other studies have related continuing use of steroids to a higher risk of developing glaucoma.
Eye Trauma
A major eye injury can also predispose you to glaucoma, especially if the injury causes an increase in your IOP. For instance, a tumor, detached retina, or lens dislocation can actually trigger glaucoma. “Injuries to the eye, such as blunt trauma and sports injuries, or a history of multiple eye surgeries for chronic eye conditions. Blunt trauma can create inflammation in the eye or alter the anatomy of the drainage system of the eye and place the patient at increased risk for development of glaucoma,” writes VisionAware.
Another source of eye trauma could be from surgery, which causes inflammation. “Usually the inflammation is limited and causes very minimal alteration of the anatomy of the drainage system of the eye. However, in rare cases, more inflammation and/or damage to the drainage structures in the eye can occur, putting the person at increased risk for glaucoma,” writes the source.
Diabetes
Diabetes is a major health problem in the U.S. It affects over 29-million Americans, according to The Glaucoma Research Foundation. There are two types of diabetes, type 1 and type 2. The most common is type 2 diabetes, which typically strikes people who are over the age of 40, overweight, and lead a sedentary lifestyle. A common complication of diabetes is diabetic eye disease, which includes diabetic retinopathy, cataracts, and glaucoma.
The Glaucoma Research Foundation writes, “The relationship between diabetes and open-angle glaucoma (the most common type of glaucoma) has intrigued researchers for years. People with diabetes are twice as likely to develop glaucoma as are non-diabetics, although some current research is beginning to call this into question.” The same goes for people who suffer from open-angle glaucoma. They are at a higher risk for developing diabetes than someone who doesn’t suffer from this eye condition.
Existing Medical Conditions
In addition to diabetes, there are other particular medical conditions that have also been linked to an increased risk of glaucoma. Mayo Clinic writes that medical conditions such as “diabetes, heart disease, high blood pressure and sickle cell anemia” are among the important risk factors for glaucoma. It also includes people who suffer from migraines.
A 2017 study published in the Journal of Optometry explained that clinical studies have found an association between low diastolic blood pressure, lower ocular perfusion pressure (OPP), and a higher risk of glaucoma.
Gender
Gender does play a role in risk for glaucoma, especially when it comes to what type of glaucoma a person will develop. There are three different types of glaucoma: open-angle glaucoma, angle-closure glaucoma, and normal-tension glaucoma. The Glaucoma Research Foundation explains that women are a whopping 50-percent more likely to develop angle-closure glaucoma than men. The reason behind this is not yet clear.
On the other hand, a 2017 study on glaucoma history and risk factors found that male gender was useful for predicting the onset of primary open-angle glaucoma. “A Bayesian meta-analysis found that men were more likely to have [open-angle glaucoma (OAG)] with the reservation that gender influence depends on the definition of glaucoma…there is no clear gender predilection for OAG,” writes the study.
Myopia
According to a study published in the Journal of Optometry, myopia is a big risk factor for glaucoma. “It is also more prevalent among Asian patients, which may help explain increased prevalence. In addition, high myopia and increased axial length in certain age groups have both been identified as risk factors suggests that the risk of glaucoma development and progression increases with the degree of myopia,” writes the source.
Other Eye-Related Risk Factors
Of course, there are a few risk factors that we should still be wary of that don’t necessarily fit into any of the categories listed above. The American Optometric Association explains that “certain features of eye anatomy, namely thinner corneas and optic nerve sensitivity, indicate an increased risk for developing glaucoma.” There are also conditions such as retinal detachment, eye tumors, and eye inflammation that can trigger glaucoma. There’s even some studies that suggest nearsightedness may also be a risk factor for glaucoma.
VisionAware points out that people with hyperopia (farsightedness) are at a higher risk for narrow-angle glaucoma, also sometimes referred to as angle-closure glaucoma or closed-angle glaucoma. Also, anyone with a corneal thickness less than 0.5 millimeters.
If Left Untreated…
It’s important to note that glaucoma will not get better on its own and it’s not something to be ignored. If you start noticing symptoms, go see an eye doctor right away. If left untreated, this condition will lead to blindness. “Even with treatment, about 15-percent of people with glaucoma become blind in at least one eye within 20-years,” writes the Mayo Clinic.