Anemia is a condition characterized by a deficiency of red blood cells, or of hemoglobin, in the blood. Hemoglobin is a protein located in red blood cells, which allows red blood cells to carry oxygen from the lungs to the rest of the human body. Anemia diminishes the capacity of the blood to carry oxygen. The element iron is needed to manufacture hemoglobin. Anemia can be temporary or long term, and it can range from mild to severe. The main causes of anemia are bleeding, hemolysis (excessive destruction of red blood cells), underproduction of red blood cells, and underproduction of normal hemoglobin.
The seven most common types of anemia are…
1. Iron Deficiency Anemia
Iron deficiency anemia is the most common type of anemia. It accounts for approximately 50-percent of the diagnosed cases of anemia. Iron deficiency anemia can result from inadequate iron intake, decreased iron absorption, increased iron demand, or increased iron loss. Symptoms of iron deficiency anemia may include fatigue, shortness of breath, chest pain, dizziness, headache, and pica (unusual cravings for substances with no nutritional value such as ice, dirt, or starch).
Blood tests such as a complete blood count (CBC) and serum ferritin level are useful for the diagnosis of iron deficiency anemia. A CBC can help determine red blood cell size, hematocrit (percentage of blood volume made up by red blood cells), and hemoglobin. Ferritin reflects iron stores and is the most accurate test to diagnose iron deficiency anemia. All of these blood tests would be decreased in iron deficiency anemia. Iron deficiency anemia is treated with iron supplementation.
2. Thalassemia
Thalassemia is a group of inherited blood disorders characterized by the body making an abnormal form of hemoglobin. It results in hemolysis, or the destruction of red blood cells. Thalassemia is more common in individuals of Mediterranean, African, and Asian descent. There are 2 main types of thalassemia, alpha and beta. Thalassemia is diagnosed using a test called hemoglobin electrophoresis.
Forms of alpha thalassemia include minor, hemoglobin H disease, and major. Alpha thalassemia major, also called hydrops fetalis, is the most severe form and causes stillbirth (death of the unborn baby during the late stages of pregnancy). Forms of beta thalassemia include minor, intermedia, and major. Beta thalassemia major, also known as Cooley’s anemia, is the most severe form and can result in severe anemia during the first year of life. Treatment of severe disease is with regular blood transfusions and in some cases bone marrow transplantation.
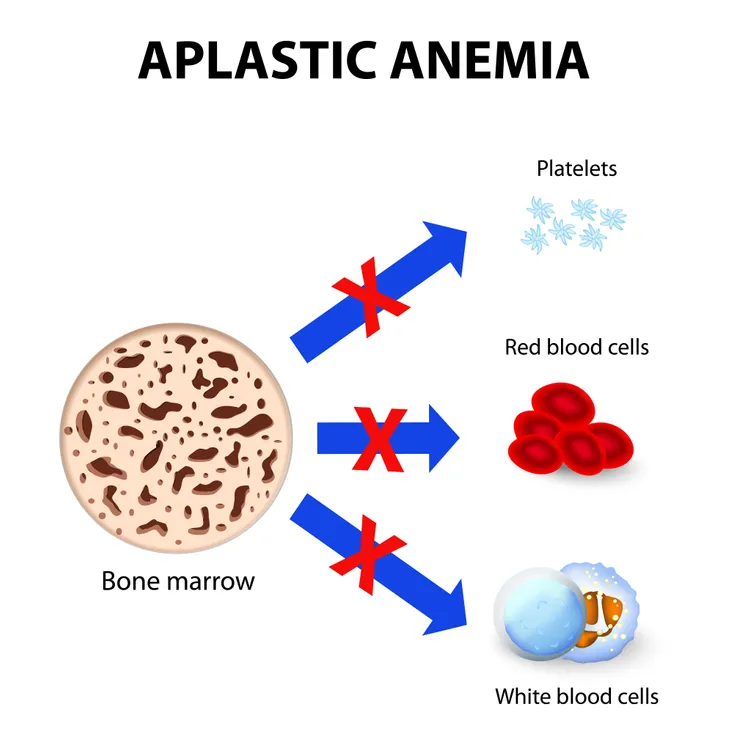
3. Aplastic Anemia
Aplastic anemia refers to a deficiency of all types of blood cells (red cells, white cells, and platelets) caused by bone marrow failure. It is a rare and serious condition that can develop at any age and can be fatal. It develops when a person’s bone marrow is injured. Factors that can temporarily or permanently injure bone marrow include radiation and/or chemotherapy treatments, exposure to toxic chemicals, certain medications (antibiotics), autoimmune disorders (lupus and rheumatoid arthritis), and certain viral infections (hepatitis, Epstein-Barr, cytomegalovirus, parvovirus B19, and HIV).
The diagnosis of aplastic anemia is confirmed with a bone marrow biopsy. Treatment of aplastic anemia may involve blood transfusions, drugs that alter or suppress the immune system (immunosuppressants), bone marrow stimulants, and bone marrow transplantation. Examples of immunosuppressants are cyclosporine (Neoral) and anti-thymocyte globulin (Thymoglobulin). Bone marrow stimulants include drugs—such as sargramostim (Leukine), filgrastim (Neupogen), pegfilgrastim (Neulasta), and epoetin alfa (Procrit).
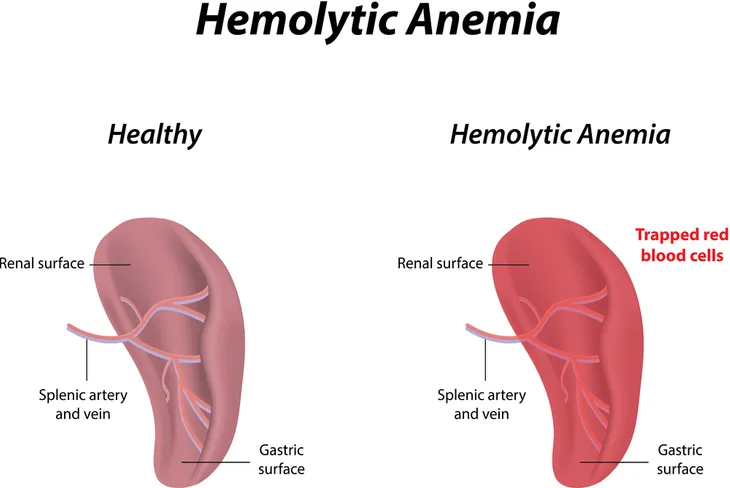
4. Hemolytic Anemia
Hemolytic anemia is a disease in which red blood cells are destroyed and removed from the bloodstream before their lifespan is over. The average lifespan of a red blood cell is 120-days. Hemolytic anemia can be inherited or acquired. Inherited means the disease is passed on due to genetic contributions from a person’s parents. Acquired means the disease develops at some point in life after birth.
Examples of inherited hemolytic anemias include spherocytosis, elliptocytosis, glucose-6-phosphate dehydrogenase (G6PD) deficiency, and pyruvate kinase deficiency. Examples of acquired hemolytic anemia include autoimmune hemolytic anemia (AIHA), mechanical hemolytic anemia, and paroxysmal nocturnal hemoglobinuria. Treatment of hemolytic anemia may involve blood transfusions, medicines (prednisone, rituximab, and cyclosporine), plasmapheresis (a procedure that removes antibodies from the blood), surgery (removal of the spleen), and bone marrow transplantation. People born with G6PD deficiency should avoid fava beans, naphthalene (a substance found in mothballs), and certain medications. People diagnosed with AIHA should try to avoid cold temperatures.
5. Sickle Cell Anemia
Sickle cell anemia is an inherited disorder of red blood cells. People with the disease have inherited two hemoglobin S genes, one from each parent. The condition is termed hemoglobin SS and leads to sickle cell anemia. In this disease, red blood cells assume a crescent, or sickle shape. Under normal circumstances red blood cells are disc shaped. The sickle shaped red blood cells can slow or block the flow of blood to body tissues and organs leading to attacks of sudden, severe pain (pain crises).
The only cure for sickle cell anemia is bone marrow transplantation. There are several effective treatments that can reduce the symptoms of sickle cell anemia. Penicillin taken 2-times per day can prevent infections. Vaccines against pneumococcus, influenza, and meningococcus can also prevent infections. Hydroxyurea taken daily can decrease the number and severity of pain crises. Blood transfusions are also utilized in the treatment of the disease.
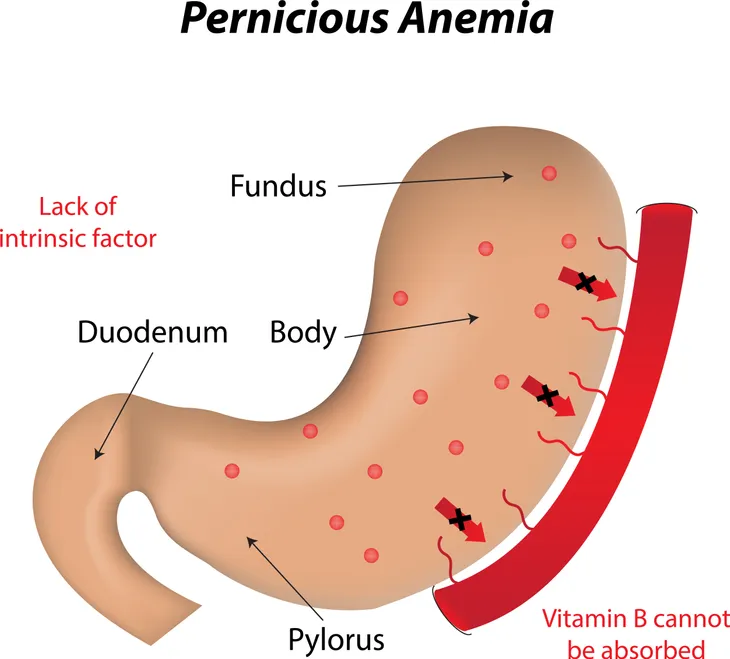
6. Pernicious Anemia
Pernicious anemia is a decrease in red blood cells that occurs when the intestines cannot properly absorb vitamin B12. The body needs vitamin B12 to make red blood cells. The intestines cannot properly absorb vitamin B12 due to a deficiency of a special protein called intrinsic factor in the stomach. The disease is more common in individuals of Celtic (English, Irish, or Scottish) or Scandinavian origin. In adults, symptoms of pernicious anemia are not seen until after age 30 and the average age at diagnosis is 60. The disease can lead to irreversible nerve damage if treatment is not initiated within 6-months of developing symptoms.
Pernicious anemia was fatal before treatment became available. Treatment of pernicious anemia may involve monthly injections, oral supplements, or nasal administration of vitamin B12. Blood transfusions are rarely required to treat the disease. There is no way to prevent pernicious anemia, but early diagnosis and treatment can help reduce complications.
7. Fanconi Anemia
Fanconi anemia (FA) is a rare, inherited blood disorder that leads to bone marrow failure. Bone marrow failure leads to decreases in all blood cells (red cells, white cells, and platelets). It occurs in all racial and ethnic groups and affects men and women equally. Individuals with Fanconi anemia are at greater risk for some cancers. Approximately 10-percent of individuals diagnosed with FA develop leukemia.
Treatment of Fanconi anemia may involve bone marrow transplantation, which can be curative. Other treatments are symptomatic and do not cure the disease. Androgen therapy can increase red blood cell and platelet counts. Androgens are a group of hormones governing male traits and reproductive activity. Over time, androgens stop working and other treatments have to be implemented. Androgen therapy can have serious side effects such as liver disease. Synthetic growth factors can increase red and white blood cell counts, without the potential for serious side effects seen with androgen therapy.