When it comes to your thyroid (the butterfly shaped gland at the front of your neck) proper functioning is a must for this gland that single-handedly regulates the secretion of hormones that manage many bodily functions, including your heart rate, body temperature, breathing, and metabolism. However, according to the Mayo Clinic, in addition to Graves or Addison’s disease, another autoimmune condition, known as Hashimoto’s disease can greatly interfere with the thyroid’s responsibilities…
1. What is Hashimoto’s Disease?
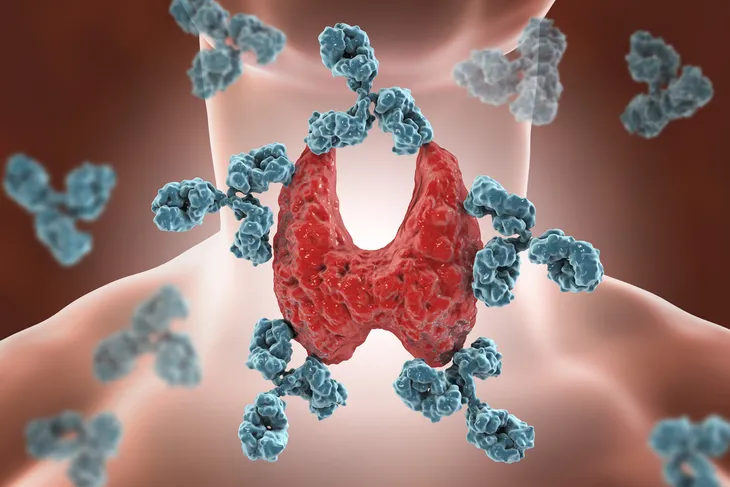
Hashimoto’s disease triggers the immune system to attack the thyroid gland, sending the endocrine system into chaos. The inflammation caused by this attack on the thyroid will typically cause hypothyroidism (or an underactive thyroid), which slows the production of thyroid hormone (also known as thyroxine or T4) and essential body functions (i.e., metabolism).
The Mayo Clinic reports that Hashimoto’s disease typically strikes middle-aged women between the ages of 30- and 50-years-old (although it can affect any gender or age group). In fact, the clinic considers it the most common cause of hypothyroidism in America.
2. Primary Symptoms of Hashimoto’s Disease
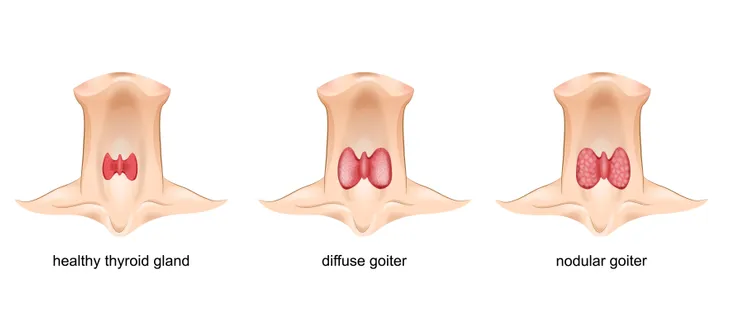
Although health experts note that the symptoms of Hashimoto’s disease are often subtle in the early stages, the first sign is often inflammation at the front of the neck, near the base just below the Adam’s apple. The swelling may be mild and gradually increase in size (known clinically as goiter), which can cause thyroid damage.
As the disease progresses, patients may start to notice symptoms associated with a decrease in thyroid hormone and an underactive thyroid gland (hypothyroidism), including puffiness in the face, unexplained weight gain, cold sensitivity, unexplained fatigue, brittle nails and hair, muscle weakness or pain, loss of memory, enlarged tongue, dry skin, constipation, lengthy periods (and heavy bleeding), and mood changes (i.g., depression).
3. Genetic Causes
According to Monika Shirodkar, MD, a board-certified endocrinologist at Jefferson Health, at Thomas Jefferson University, autoimmune diseases, such as Hashimoto’s disease, are often genetic in nature.
In fact, Dr. Shirodkar explains that if you have a family history of thyroid disease or any autoimmune disorders (i.g., lupus, rheumatoid arthritis, Crohn’s disease ,or celiac disease), you are at increased risk of developing another autoimmune condition.
4. Non-Genetic Causes
Many other health conditions can affect thyroid function, and vice versa. For instance, as the Mayo Clinic notes, existing hypothyroidism can crop up in issues like high blood cholesterol.
In addition, certain medical procedures can also impact or even damage the thyroid, including radiation therapy (particularly to the upper chest, neck, or head areas), treatments with radioactive iodine or anti-thyroid medications, and thyroid surgery. Also, excessive environmental radiation exposure can increase your chances of developing Hashimoto’s disease.
5. Testing and Diagnosing Hashimoto’s Disease
Your family doctor may suspect Hashimoto’s disease if you complain about unexplained fatigue or sluggishness, appearance of a goiter, constipation, or unexplained weight gain.
Typically, doctors will order a blood test to check your thyroid hormone (T4) and thyroid-stimulating hormone (TSH) levels, as well as if any antithyroid antibodies (TPO antibodies) are present, which may indicate an autoimmune disorder.
6. Treating Hashimoto’s Disease with Synthetic Hormones
If your blood tests reveal thyroid hormone deficiency, your doctor may prescribe oral synthetic hormone replacement therapy (i.e., levothyroxine [Synthroid or Levoxyl]) to simulate the natural thyroxine hormone that is produced by a healthy thyroid gland.
The synthetic hormones are meant to re-establish healthy hormone levels and right the bodily havoc (i.g., slow metabolism, constipation, dry skin, and energy loss) caused by hypothyroidism. Doctors typically test and adjust your TSH level as necessary, in 6-8 weeks at the outset to every 12 months for stable levels. No side effects should occur while you’re taking the adequate dosage of synthetic thyroid hormone; however, you may need to take it for the remainder of your life.
7. Natural Therapies for Hashimoto’s Disease
As Hashimoto’s disease patients adjust to their medication, it may take some time for symptoms to normalize. You can also try a few natural therapies to help ease symptoms if you are taking medication or if the thyroid hormone level is only borderline low and you don’t require synthetic hormones.
However, Dr. Raphael Kellman, author of The Microbiome Diet and the founder of the Kellman Center for Integrative and Functional Medicine, establishes a clear link between gluten consumption and Hashimoto’s disease. However, Dr. Shirodkar cautions that any natural remedies, including dietary changes (i.e., cutting out eggs, gluten-containing foods, peanut butter, and soy), and taking probiotics should be administered under the guidance of an integrative health center along with your doctor’s knowledge.