Rheumatoid arthritis sufferers know joint pain all too well—it’s a condition that causes swelling and stiffness around the joints, making movement difficult and often excruciating. For relief, many rheumatoid arthritis sufferers reach for over-the-counter pain medications.
But properly treating rheumatoid arthritis takes more than this. It requires a deep understanding of the condition, including its causes. Through such an understanding, one can begin to learn how the condition can be treated over the long term and how alternative treatments—including those that don’t involve prescription or over-the-counter drugs—can help alleviate joint pain. So, what, exactly, do you need to know about rheumatoid arthritis?
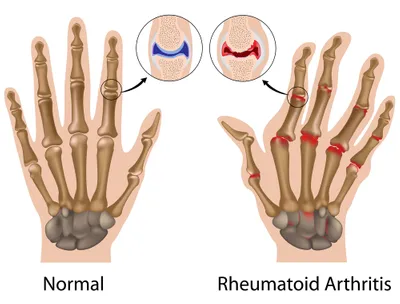
1. RA Targets the Joints
Rheumatoid arthritis is a condition that takes aim at the body’s many joints, and particularly those in the hands, knees, and feet. According to the University of Maryland Medical Center, rarely does it target just a single joint, though, meaning that people experiencing rheumatoid arthritis in one part of the body often feel it in a completely different part of the body, too.
That said, not all people suffering from rheumatoid arthritis are crippled by the condition. Those with mild rheumatoid arthritis may have occasional flare-ups of pain that can be overcome with over-the-counter pain medications, such as Aleve. However, those suffering from moderate or extreme versions of the condition will have more symptoms, such as regularly feeling sick and tired or even getting fevers.
2. Anyone Can Develop RA
Generally speaking, significant joint pain is associated with people of an advanced age—such as individuals in their post-retirement years. However, rheumatoid arthritis does not discriminate based on age. In fact, anyone can suffer from the condition, even children and young adults.
That said, research from the CDC notes that rheumatoid arthritis is more prevalent in older and middle age people. It is also slightly more prevalent in women than men. Nevertheless, one should not rule out the possibility that they may have rheumatoid arthritis based on their age or gender. If you think you may be suffering from rheumatoid arthritis, talk to your doctor as soon as possible.
3. RA Continues to Stump Doctors
Rheumatoid arthritis may be one of the most common conditions that continues to puzzle physicians and other medical experts around the world. To this day no one has clearly determined what, exactly, causes rheumatoid arthritis. What we do know is that the condition arises when an individual’s immune system begins to attack their own body tissues, particularly those around the joints. However, experts still don’t know what causes the body to do this to itself.
That said, experts do know that there are a number of factors that influence one’s chances of developing rheumatoid arthritis. Genetics plays an important part, meaning you may be vulnerable if someone in your family suffers from the condition. Doctors also believe one’s environment and their hormones may also be factors.
4. A Diagnosis is a Complex Affair
Many health conditions are relatively easy to diagnose, requiring only a sample of some bodily fluid (such as saliva, urine, or blood). But rheumatoid arthritis is not one of those conditions: in fact, it can be downright difficult to diagnose, and may require several long visits to a few different types of specialists.
According to the Mayo Clinic there’s no single test that can positively identify rheumatoid arthritis in an individual. Another problem is that the symptoms of rheumatoid arthritis are similar to those seen with other types of joint disease. On top of that, the complete symptoms of rheumatoid arthritis can take a long time to develop—perhaps even a few years. That’s why doctors look at a variety of factors—from medical history to genes to physical exam and x-rays—in order to make a rheumatoid arthritis diagnosis.
5. There are Many Ways to Treat RA
There is no single way to treat rheumatoid arthritis. Like many other painful health conditions, there are several approaches to alleviating pain, reducing swelling around the joints, and helping patients lead normal lives.
The first step is to educate the patient on the disease through self-management programs and support groups. Next steps include showing the patient how various physical exercises can help to strengthen the muscles around the joints and help to reduce inflammation and pain. Doctors may also prescribe anti-inflammatory medications designed to reduce pain and help individuals gain an upper hand on the disease.
6. Diet and Exercise Can Help
Those who are diagnosed with rheumatoid arthritis will be encouraged to watch their weight, to exercise regularly, and to follow a healthy diet. That’s because being in good shape can help reduce the amount of weight being placed on the joints, thereby limiting inflammation and the pain that comes with rheumatoid arthritis.
That means exercise is a critical part of treating the disease, according to studies from the National Institutes of Health. However, that doesn’t mean one should engage in intense exercise routines—such as interval training or running—all the time. Moderate exercise, such as cycling or going for a walk can also be very helpful. Before starting your own training regime designed to help alleviate the symptoms associated with rheumatoid arthritis, be sure to consult your doctor.