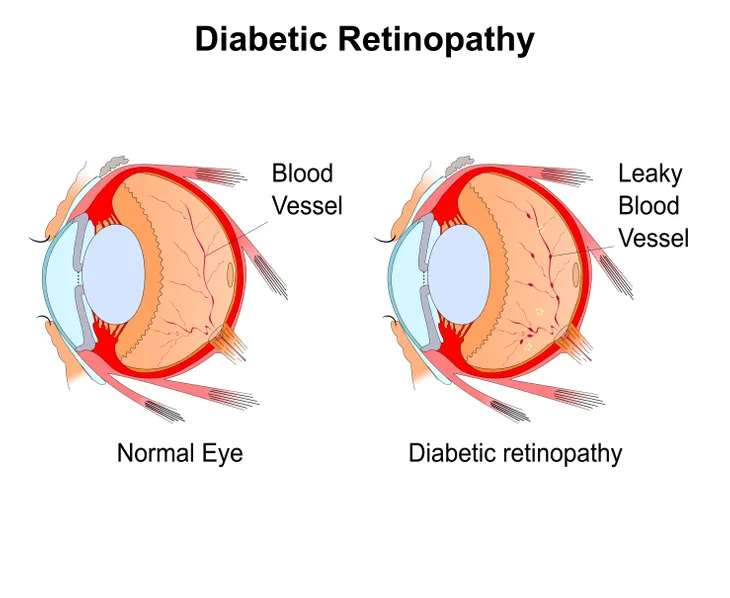
For those with diabetes, both type 1 and type 2, there is a risk of developing an eye condition called diabetic retinopathy. According to the Mayo Clinic, it is caused “by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina).”
The likelihood of developing diabetic retinopathy increases the longer a person has diabetes, especially if their blood sugar is chronically high. While symptoms of this eye complication may be slow to develop, it is possible for it to eventually cause blindness. Read on to learn more about the signs, causes, and risk factors of diabetic retinopathy, as well as what can be done to prevent it from occurring altogether.
Signs
As previously mentioned, symptoms may not occur in the early stages of diabetic retinopathy. As the disease progresses, however, you may experience a variety of vision-related issues. These issues can include blurred vision, an inability to see colors, having dark or empty areas in your field of view, and sudden vision loss (oftentimes while reading or driving).
According to the Mayo Clinic, another common symptom is seeing “spots or dark strings floating in your vision.” These are known as “floaters” and are caused by bleeding from abnormal retinal blood vessels. The National Eye Institute says, “These spots sometimes clear on their own. But without prompt treatment, bleeding often recurs, increasing the risk of permanent vision loss.”
Causes
When blood sugar levels are consistently high over a long period of time, it can cause the tiny blood vessels that maintain retina health to become blocked. WebMD says the eye “will try to grow new blood vessels, but they won’t develop well,” leading them to “leak blood and fluid into your retina.”
As the condition progresses and more blood vessels become blocked, the source adds that “[s]car tissue builds up because of all the new blood vessels your eye has grown.” As a result of the pressure exerted by the scar tissue, the retina can detach. Other issues such as glaucoma may also occur.
Risk Factors
As mentioned earlier, anyone with type 1, type 2, or even gestational diabetes is at risk of developing diabetic retinopathy. This risk only increases the longer a person has diabetes, especially if they struggle to control their blood sugar levels.
According to the Mayo Clinic, other risk factors that increase the likelihood of developing this eye complication include high blood pressure (hypertension), high cholesterol, smoking, and a person’s ethnicity (people who are African-American, Hispanic, or Native American have a greater risk).
Diagnosis
Diabetic retinopathy is diagnosed during a comprehensive eye exam. As one component of this exam, an optometrist will place drops in the eyes that dilate the pupils in order to better examine the retina and ocular nerve for abnormalities, scar tissue, or bleeding.
Other testing may including retinal photography or tomography, which the American Optometric Association says is to “document [the] current status of the retina,” or fluorescein angiography, which is done to “evaluate abnormal blood vessel growth.”
Treatment
A person’s treatment options are largely dependent on the type and severity of their diabetic retinopathy. Treatment is not usually recommended during the early stages of the condition, as vision has not yet been compromised. Once it becomes advanced, however, there are three primary treatment options that are used to help prevent vision from worsening.
The first is scatter laser treatment, which the CNIB says involves “a large number of microscopic thermal laser burns in the retina to shrink abnormal blood vessels.” The second option is vitrectomy, where “vitreous gel is replaced with a salt solution that mimics the normal fluids of the eye.” This treatment must be done if blood leaks into the center of the eye. Finally, there are intraocular (anti-vascular endothelial growth factor [VEGF]) injections, which are “injected into the eye to stop the growth of abnormal blood vessels.”
Prevention
There are a variety of different things that a person can do to reduce their risk of developing diabetic retinopathy, including having regular eye examinations by an optometrist. WebMD recommends going at least once per year, and women with diabetes who become pregnant should have an exam during the first trimester.
In addition to regular eye examinations, properly managing and maintaining blood glucose levels, blood pressure, and blood cholesterol is crucial. To do this, AllAboutVision.com suggests eating a healthy diet, exercising regularly, and refraining from tobacco use.