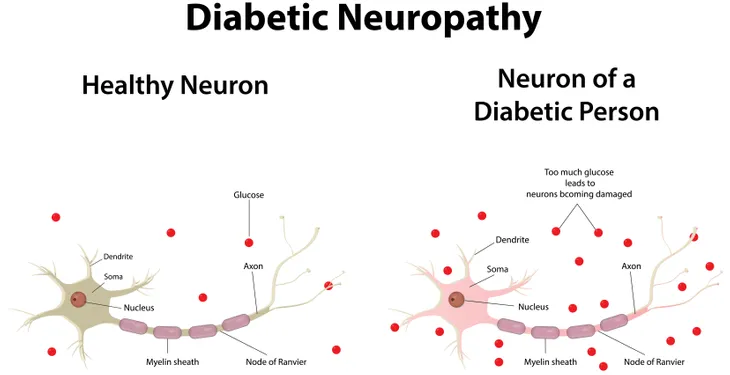
Diabetic neuropathy is a nerve disorder that can occur in people with type 1 or type 2 diabetes. It is commonly caused by blood sugar levels being too high over a prolonged period of time, resulting in nerve damage throughout the body, most frequently in the legs and feet.
The National Institute of Diabetes and Digestive and Kidney Diseases says, “About 60 to 70 percent of people with diabetes have some form of neuropathy,” but the risk is especially high for those who have had diabetes for over 25 years. Read on to learn more about the different types of diabetic neuropathy, the symptoms to look out for, and the treatment options that are available.
Types
The family of diabetic neuropathies is made up of the following four main types: peripheral, autonomic, proximal, and focal. According to MedicalNewsToday.com, peripheral neuropathy is the most common form and affects the nerves of the hands and feet, while autonomic neuropathy affects “the nerves that control the involuntary functions of the body,” including digestion, bowel and bladder function, and perspiration.
The National Institute of Diabetes and Digestive and Kidney Diseases adds that it can also impact the nerves “that serve the heart and control blood pressure, as well as nerves in the lungs and eyes.” Proximal neuropathy, on the other hand, “causes pain in the thighs, hips, or buttocks and leads to weakness in the legs.” Finally, focal neuropathy is when one nerve or a group of nerves anywhere in the body experience sudden weakness.
Symptoms
The signs and symptoms associated with diabetic neuropathy are largely dependent on which type of the disorder a person has. With peripheral neuropathy, they may experience numbness or tingling in their arms or legs, as well as pain or cramping in these areas. If the individual has autonomic neuropathy, Healthline.com says constipation, trouble swallowing and gastroparesis are common.
Symptoms of proximal neuropathy include sudden, sharp pain in the hip, thigh, or buttock, typically only on one side of the body, as well as weakened muscles that can make it difficult to go from a seated to standing position. With focal neuropathy, a person may struggle to focus or have double vision, or they may experience facial paralysis in one side of the face, which is known as Bell’s palsy.
Causes/Risk Factors
As mentioned earlier, when blood glucose (sugar) levels are too high for too long, it can lead to diabetic neuropathy. One reason it is thought to cause this nerve damage is because “high blood sugar interferes with the ability of the nerves to transmit signals,” says the Mayo Clinic. The source adds that “It also weakens the walls of the small blood vessels (capillaries) that supply the nerves with oxygen and nutrients.”
High blood sugar isn’t the only cause of diabetic neuropathy. The Canadian Diabetes Association says that other risk factors include elevated triglycerides, excess body weight, smoking, and high blood pressure.
Diagnosis
Diabetic neuropathy is often diagnosed based on a person’s symptoms, and the results of a variety of physical exams. When testing for peripheral neuropathy, for instance, the doctor may conduct a filament test where a thin nylon rod is pressed against different areas of the feet to test sensitivity to touch.
Other tests include nerve conduction studies, which “check the transmission of electrical current through a nerve,” and electromyography, which “shows how well muscles respond to electrical signals transmitted by nearby nerves,” says the National Institute of Diabetes and Digestive and Kidney Diseases.
Treatment
As there is no known cure for diabetic neuropathy, treatment is intended to help slow the disease’s progression. To do this, MedicalNewsToday.com says the first step is to “get blood sugars under control and to manage high blood pressure and cholesterol levels.” Not only can this delay or prevent certain symptoms but also it may improve those a person currently has.
To help relieve some of the pain associated with the disorder, a doctor may recommend taking certain drugs such as duloxetine (Cymbalta), pregabalin (Lyrica), and gabapentin (Neurontin). Along with such medications, the source says physical therapy can also help to “alleviate pain, burning, and tingling sensations in the legs and feet,” as well as help with muscle cramps and weakness.
Prevention
According to Healthline.com, “Diabetic neuropathy is preventable if you manage your blood sugar levels properly.” To do this, the source recommends consistent monitoring, taking prescribed medications, eating healthy, and being physically active.
Maintaining proper foot care is also essential. The Mayo Clinic suggests having a comprehensive foot exam at least once per year, and taking good care of them at home. This includes examining the feet each day for sores or irritation, trimming nails regularly, and keeping them clean and dry.