According to the Alzheimer’s Association, normal pressure hydrocephalus (NPH) is “a brain disorder in which excess cerebrospinal fluid accumulates in the brain’s ventricles,” causing dementia and other symptoms.
It is a fairly rare condition, affecting approximately 700,000 people in the United States, most of whom are over the age of 60. Although, many more people may have NPH and go undiagnosed, as its symptoms are similar to other neurological diseases. Let’s get to know the specifics of this disorder by exploring these five facts about NPH—including causes, symptoms and available treatment options.
1. Risk Factors and Causes
As with many medical conditions, the risk of developing NPH increases as a person gets older, particularly after they reach the age of 60. But that isn’t the only risk factor that can increase a person’s likelihood of developing the condition. According to Healthline.com, other factors include cerebrovascular disease, vascular disorders, hypertension, and Alzheimer’s disease.
Unfortunately, the exact cause of NPH is rarely ever known. However, there are certain conditions that may cause it to occur, including a head injury, stroke, meningitis, brain tumor, or surgery on the brain, although WebMD says that it is not clear how they lead to NPH.
2. Symptoms
NPH is characterized by three primary symptoms. The first is difficulty walking, also known as gait disturbance. The individual may struggle to lift their feet off the ground when walking, and “tend to walk with their legs wide apart and their body bent forward,” according to the Alzheimer Society.
The second main symptom is dementia, which includes forgetfulness, short-term memory loss, apathy, struggles with planning and decision-making, and changes in personality or behavior. The third symptom is a loss of bladder control, which the Alzheimer’s Association says “tends to appear somewhat later in the disease.”
3. Diagnosis
As mentioned earlier, diagnosing NPH can be challenging because its symptoms are similar to those of other neurological diseases. There are, however, several tests that a neurologist may conduct to help with the diagnosis. A clinical exam is often the first, which the Hydrocephalus Association says “consists of an interview and/or physical/neurological examination.”
The physician may then order a magnetic resonance imaging (MRI) or computerized tomography (CT) scan of the brain to help detect the enlarged ventricles that are characteristic of NPH. Additionally, a lumbar puncture (also known as a spinal tap) may also be needed. According to WebMD, this procedure involves the removal of some cerebrospinal fluid from the lower back in order to analyze it for “abnormalities that might give a clue as to the problem.”
4. Treatment
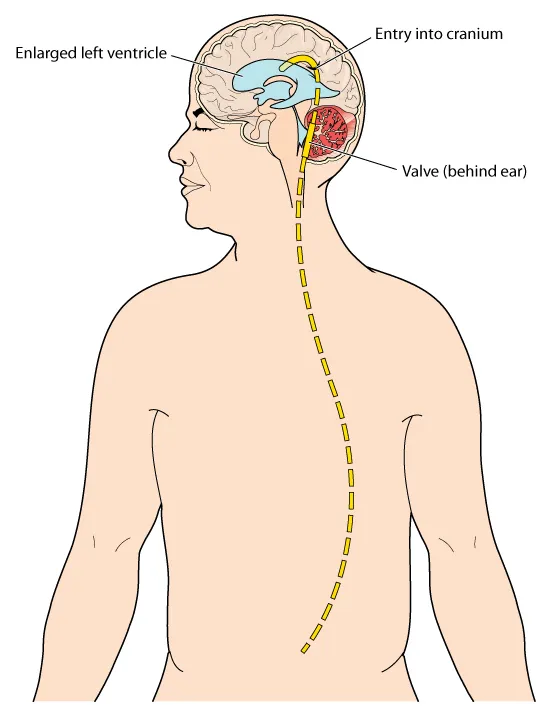
The primary treatment option for NPH is ventricular shunting, which involves having a long, thin tube inserted into the brain to drain the excess fluid. The most common type used is a ventriculoperitoneal (VP) shunt, which goes from the brain to the abdomen, where the body absorbs the fluid.
The Alzheimer Society says this procedure is “most likely to help improve the walking abilities of a person with NPH,” although it’s possible for symptoms related to dementia and bladder control to improve as well.
5. Outlook
As NPH is a progressive condition, its symptoms will worsen over time if not effectively treated. But a person’s treatment options largely depend on whether or not he or she is a candidate for receiving a ventricular shunt.
While approximately 70-percent of people’s symptoms improve after the surgery, the remaining individuals do not. As a shunt remains the only effective treatment option for the condition, few options remain for those who are not able to have the procedure or for those whom the surgery was not effective.