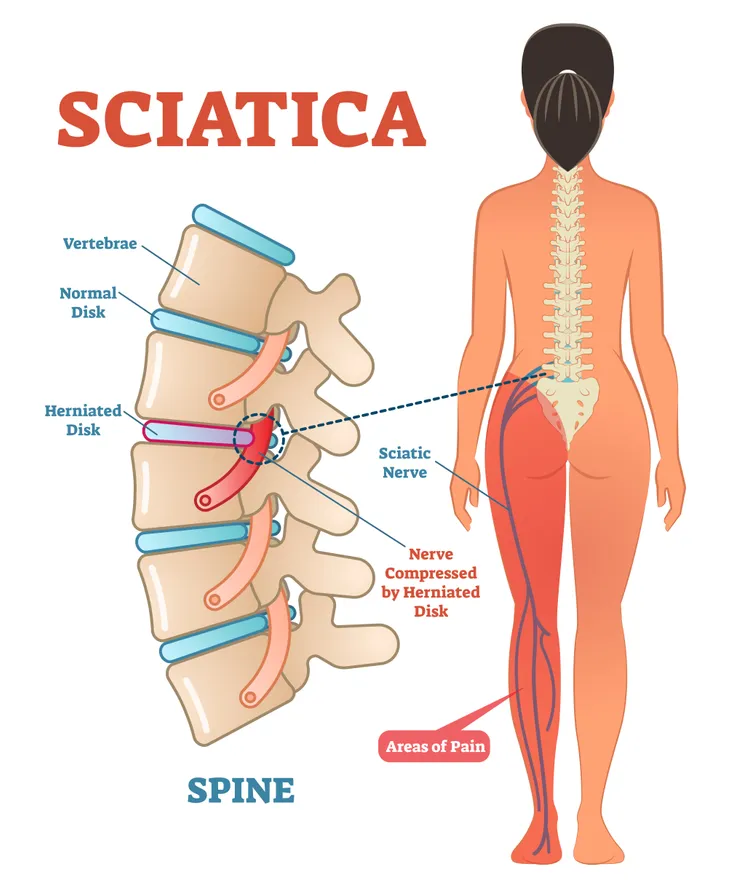
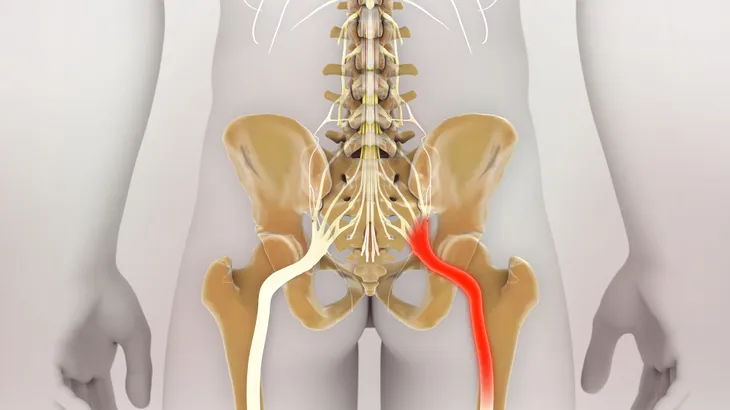
Specialists at Cleveland Clinic’s Center for Spine Health, characterize sciatica as several symptoms rather than a diagnosis. Sciatica can cause numbness, tingling, and shooting pain—usually centered in the areas of the buttocks and lower hips—that reverberates all the way through the toes. This is because the sciatic nerve itself extends from the lower back, near the spine, and branches out in roots from the lumbar spine, along the pelvis, deep into each buttock, and directly down each leg.
Experts link sciatica to nerve pain, which is either due to a pinched nerve, slipped disk, or herniated disk. However, pain in the longest and widest single nerve in the body is just one symptom of sciatica.
Here are five telltale symptoms of sciatica…
1. Sciatic Pain
The most obvious and reported symptom of sciatica is a jolting pain (akin to an electric shock) that begins when you cough, sneeze, or sit for prolonged durations on one side of the body. This pain can be traced back to pressure from a pinched nerve —again, likely due to a herniated (ruptured) or slipped disk, spinal stenosis, degenerative disc disease, spondylolisthesis (displacement of a vertebra as compared to another), or other pressure-causing issues in the vertebrae (bones of the spinal column) that come into contact with the sciatic nerve. However, patients can easily mistake nerve pain, such as sciatica, for muscle-associated pain following an injury or strain to the muscles and ligaments supporting the back.
For instance, according to researchers from Harvard Medical School, an injury to a muscle located deep in the buttocks known as the piriformis can often cause muscles there to shorten and tighten. If this occurs, oftentimes the muscle swells and constricts, because it’s unable to receive the proper nutrients via blood flow. To check for muscle shortening (as opposed to sciatica) in the lower back, apply strong pressure with the fingers for 10-seconds as you press into the tense or knotted area. When you press, you should feel pain reverberate throughout the entire body.
2. Loss of Bowel and Bladder Function
As opposed to you drinking too much herbal tea before bedtime and having to wake up frequently to relieve yourself mid-slumber, sciatica can place pressure on the nerves surrounding the bowel and bladder, causing you to suddenly lose control.
Doctors at the American Academy of Orthopedic Surgeons claim that complete bowel and bladder loss will cause spontaneous and embarrassing movements and is treated as an emergency situation that may require surgery. Although complete loss of bowel and bladder control is rare, it can happen and cause permanent damage to the bladder and bowels when the spinal canal places excessive pressure on the surrounding nerves.
3. Inflammation and Swelling
Inflammation often accompanies sciatic pain. If the sciatic nerve pain and swelling doesn’t improve within a 90-day (or 3-month) timeframe, medical experts will often prescribe a combination of anti-inflammatories, pain relievers, and physiotherapy to reduce the pressure and move the displaced disk back into its rightful place.
According to research from the Cleveland Clinic, sciatic pain will typically resolve on its own (i.e., re-positioning of the disk and removing pressure from nerves) in roughly 80-percent of cases. However, if your sciatic pain doesn’t improve by the 3-month mark, you should seek medical attention and explore medication relief options.
4. Weakness in Just One Leg
According to research published by the U.S. National Library of Medicine, pain or weakness in a single leg (not both) is a red flag for sciatica. Since the sciatic nerve is the longest single nerve in the body, doctors can pinpoint it as a potential issue in patients that experience weakness in one leg and not the other.
The weakness can occur at any point in the sciatic nerve, which starts at the lower spine and spans the leg down to the foot. If the sciatic nerve is pinched or compressed at any point, nerve function becomes compromised, and spasms, numbness, “pins and needles” sensation, prickling, and weakness can occur in the region of the buttocks or span any section of a single leg. Progressive weakness is a clear sign of a neurological (nerve) issue.
5. Progressive Sciatica Symptoms
The Mayo Clinic indicates that cases of mild sciatica are typically temporary and right themselves over time. However, if any of the above symptoms progress from mild to worse or if the pain worsens over a week, it’s time to seek immediate care.
The Mayo Clinic points to progressive and severe pain in the lower back or leg accompanied by muscle weakness and numbness as a major cause for concern. If you’re unable to control bladder or bowel function, you should also consider your case an emergency. Following any sort of severe injury (i.g., automobile accident) it’s wise to follow up with your doctor and be examined for sciatica.