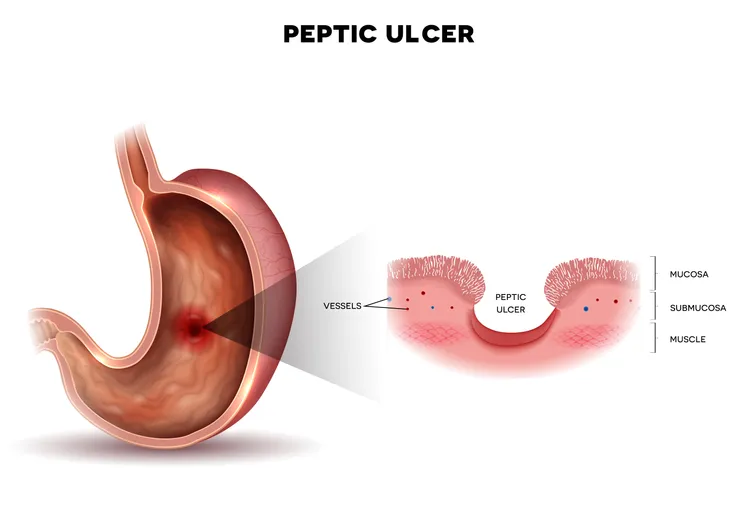
Peptic ulcers are “sores that develop in the lining of the stomach, lower esophagus, or small intestine,” defines Healthline.com, and they occur as a result of the stomach’s mucus lining no longer working effectively.
Peptic ulcers are a common issue, affecting approximately 1 in 10 people in Western countries at some point in their lives, and they can cause symptoms such as burning stomach pain, nausea, and loss of appetite. But what is it that causes peptic ulcers to occur in the first place? The following are the five most common culprits.
Bacterial Infection
An infection with the bacteria Helicobacter pylori is the primary cause of peptic ulcers. The Mayo Clinic explains that these bacteria “commonly live in the mucus layer that covers and protects tissues that line the stomach and small intestine.”
While they don’t regularly cause issues, they can sometimes trigger “inflammation of the stomach’s inner layer, producing an ulcer.” It is thought that some of the primary ways H. pylori spreads is through food, water, and close person-to-person contact.
Frequent Use of NSAIDs
The second most common cause of peptic ulcers is the overuse of nonsteroidal anti-inflammatory drugs (NSAIDs). These include common over-the-counter medications such as aspirin, ibuprofen, and naproxen.
When used on a chronic basis for weeks or months at a time, MedicineNet.com says that NSAIDs can interfere with the production of prostaglandins, “substances which are important in helping the linings of the esophagus, stomach, and duodenum resist damage by the acidic digestive juices of the stomach.” Therefore, a reduced amount of prostaglandins makes the stomach more susceptible to ulcers.
Smoking
Not only can smoking increase a person’s risk of developing peptic ulcers, especially in those who are infected with H. pylori but also, as MedicineNet.com explains, the unhealthy habit can “increases the risk of complications from ulcers, such as ulcer bleeding, stomach obstruction, and perforation.”
On top of that, the source says that smoking is “a leading cause of failure of treatment for ulcers.” So, in addition to causing peptic ulcers and the complications associated with them, smoking actually prevents them from healing.
Zollinger-Ellison Syndrome
Peptic ulcers may also occur due to a rare condition called Zollinger-Ellison syndrome. With this disease, WebMD explains that tumors in the pancreas “secrete large amounts of a hormone called gastrin,” and gastrin “signals the stomach to produce more acid.”
This overproduction of stomach acid eventually damages the lining of the stomach, making it highly susceptible to ulcers. In fact, the source says that a whopping 90 to 95 percent of people with Zollinger-Ellison syndrome will develop peptic ulcers “at some point during their lives.”
Other Causes
There are a variety of other factors that have been linked with the development of peptic ulcers. When taken alongside NSAIDs, the Mayo Clinic indicates that certain medications can “greatly increase the chance of developing ulcers.” These include steroids, anticoagulants, low-dose aspirin, selective serotonin reuptake inhibitors (SSRIs), alendronate (Fosamax), and risedronate (Actonel).
MedicalNewsToday.com adds that excess stomach acidity, also known as hyperacidity, is a known culprit and can occur due to “genetics, smoking, stress, and some foods.” Alcohol consumption has also been known to cause peptic ulcers, as the Mayo Clinic explains that it “can irritate and erode the mucus lining of your stomach, and it increases the amount of stomach acid that’s produced.”