If you have a disorder affecting the lower end of your digestive system, you may have been diagnosed with a condition known as inflammatory bowel disease (IBD). Typically, this diagnosis occurs after an examination by a medical professional which reveals significant and chronic inflammation of the lower intestine, although sometimes, IBD can also involve inflammation of other parts of the digestive tract. There are two main types of IBD: ulcerative colitis and Crohn’s disease. The former involves the development of painful ulcers (sores) in the large intestine and rectum, while the latter usually refers to the emergence of significant inflammation beyond the lining of the bowel. Both conditions tend to result in diarrhea (sometimes bloody), pain, exhaustion, and may lead to weight loss.
This leaves any individual who feels they may have IBD wondering how medical professionals will examine them in order to determine the exact nature of their condition. Now, let’s take a look at the various tests experts will use in order to arrive at an accurate diagnosis.
Blood Test
A blood test is one of the least invasive and therefore earliest tests a doctor will run to determine if an individual is suffering from IBD. A blood test can help with the diagnosis by showing if the patient has anemia, which occurs when there are insufficient red blood cells to pass enough oxygen to the body’s tissues.
Should anemia be detected, this could be a sign that the patient is suffering from a form of IBD. Unfortunately, a blood test cannot immediately reveal the presence of IBD, which means further tests will need to be run. In some cases, failure to find anemia may lead medical experts to cease their search for IBD or consider other possibilities.
Fecal Occult Blood Test
Like a standard blood test, the fecal occult blood test is a non-invasive test that can reveal signs of IBD. In this test, medical professionals will be looking for signs of blood hidden inside a patient’s stool.
Should blood be found in the patient’s stool, this could be a sign of the presence of some problem affecting the lower intestine or rectum. However, because there are a variety of conditions that can result in blood in the stool, this is not a definitive sign of IBD and will likely be followed by other tests.
Colonoscopy
Unlike the standard blood test and fecal occult blood test, colonoscopy is a more invasive procedure that’s often used by doctors to directly examine the entire lower intestine and rectum in order to find signs of IBD.
The exam involves a doctor using a long, narrow, and highly flexible camera to examine the bowel lining, including any inflammation or sores affecting that tissue. The physician may also use a colonoscopy to take small tissue samples (biopsies)that can be tested to determine if an IBD-related condition is present.
Flexible Sigmoidoscopy
Flexible sigmoidoscopy is similar to colonoscopy but is actually less invasive. As with the colonoscopy, a slim, flexible camera is used for the examination, but the focus is primarily on the lower part of the one-third of the lower intestine, known as the sigmoid colon and rectum.
Why would your doctor use flexible sigmoidoscopy instead of a full colonoscopy? Primarily because the lower intestine is clearly inflamed and painful, which could make a colonoscopy too damaging and uncomfortable for the patient. For this reason, it’s possible flexible sigmoidoscopy could be used in cases where a diagnosis of IBD has already been made.
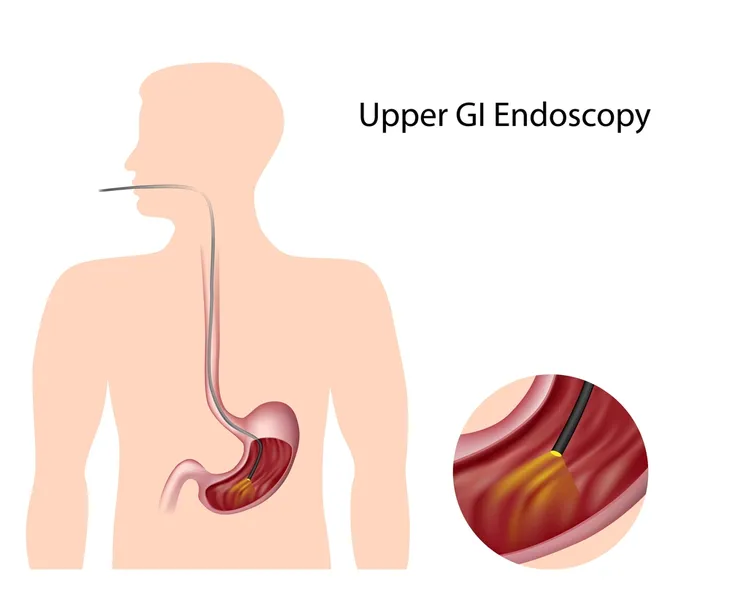
Upper Endoscopy
Upper endoscopy is, like the colonoscopy, a fairly invasive procedure but focuses on the esophagus, stomach, and small intestine instead of the lower intestine and rectum. Also, like the colonoscopy, a long, thin and highly flexible camera is used to examine tissue, although in this case it’s used through the mouth and throat instead of the anus/rectum.
Upper endoscopy will not be used in all cases where IBD, is detected. It is primarily employed when the patient has been diagnosed with Crohn’s disease, which can manifest in the upper section of the digestive tract, as well as the lower intestine and rectum. It is typically used when the patient, in addition to abdominal pain and diarrhea, is experiencing upset stomach, vomiting, and pain in the upper abdomen.
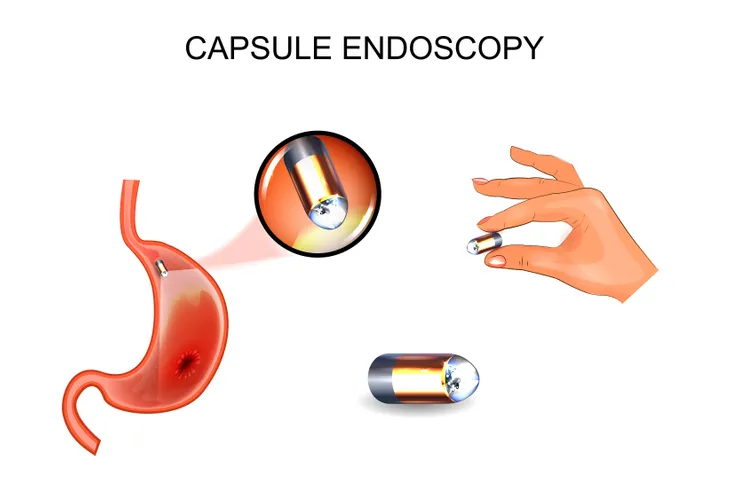
Capsule Endoscopy
As the name suggests, capsule endoscopy is similar to upper endoscopy but involves the use of a capsule that actually contains a wireless camera. Once this capsule is consumed by the patient, images of the digestive system, including the esophagus, stomach, small intestine, and large intestine, are sent to a recorder that’s typically worn by the patient. Once the capsule leaves the body through the stool, it can be retrieved and used by physicians to confirm or rule out a diagnosis of IBD.
Should evidence of IBD be found using capsule endoscopy, doctors may recommend the patient undergo another test, such as colonoscopy. Should signs of IBD show that the lower intestine is particularly inflamed, the following test may instead be flexible sigmoidoscopy.
Balloon-Assisted Enteroscopy
Balloon-assisted enteroscopy is a type of diagnostic test used when other tests, such as the capsule endoscopy, fail to produce a definitive diagnosis regarding IBD.
It involves using a scope connected to a device known as an “overtube,” which together can help a physician take a closer look at the small intestine. Typically, an endoscope won’t provide a doctor with a sufficient view of this area, although capsule endoscopy can reveal abnormalities warranting further examination.
X-Ray
The standard x-ray offers a relatively simple and less invasive way to determine if a patient’s abdominal pain is resulting from more serious issues, such as the perforation of the colon.
Should such a serious problem be discovered, physicians will follow a different course of action than they might proceed along if a condition associated with IBD, such as Crohn’s disease or ulcerative colitis, is detected. Whereas suspicion of IBD may lead to tests, such as capsule endoscopy or colonoscopy, a serious concern revealed by X-ray may lead to more dramatic steps, such as scheduling surgery.
Computerized Tomography (CT) Scan
Should your doctor desire more detail than can be provided by ya standard X-ray, they may require you to undergo a CT scan. Unlike the typical X-ray, the CT scan can show your doctor how the entire bowel looks, including the state of the tissue lining the lower intestine.
In addition to the CT scan, doctors may use CT enterography, which is an even more niche form of scan that can provide some of the clearest images of the small intestine currently available. Today, it has largely eclipsed the barium X-ray in the medical professions focused on digestive health.
Magnetic Resonance Imaging (MRI)
You’ve probably heard of MRI since it’s often discussed in relation to sports injuries affecting professional athletes. An MRI machine employs a magnetic field and radio waves to provide a doctor with a clear picture of the organs and tissues of a selected part of the body.
The advantage of the MRI is that, unlike a CT scan, it doesn’t expose the patient to any radiation. The drawback of the MRI is that its application is somewhat limited, with doctors mostly using it to focus their examination on the area around the anus.
Dietary Changes
One of the first changes a doctor will make to determine if IBD is an issue can involve a range of changes to the diet. By eliminating or adding certain foods, your doctor can get a more detailed idea of the issue causing abdominal pain or diarrhea.
The result of these dietary changes may help your doctor determine the appropriate next step for your therapy. Should the dietary changes result in an alleviation of the most concerning symptoms, no further tests may be required.
Lifestyle Changes
In addition to making some significant changes to your diet, a doctor may recommend certain lifestyle adjustments before moving on to more invasive and involved diagnostic tests, such as the CT scan or colonoscopy.
Some of these lifestyle changes may include getting a certain type of exercise or cutting back on certain behaviors, such as smoking cigarettes or excessively drinking alcohol. Depending on how the patient reacts to these changes, a doctor can then develop a plan for proceeding with further tests.