Abdominal pain is a common ailment that just about everyone will experience at least once in his or her lifetime. Pain in the left lower side of the abdomen is referred to as left lower quadrant (LLQ) pain. It can arise in the digestive tract, skin, abdominal wall muscles, urinary tract, blood vessels, or male and female reproductive organs. Important clues in the diagnosis of LLQ pain would be the characteristics of the pain and any accompanying signs or symptoms.
The 12 common causes of left lower quadrant pain in men and women are…
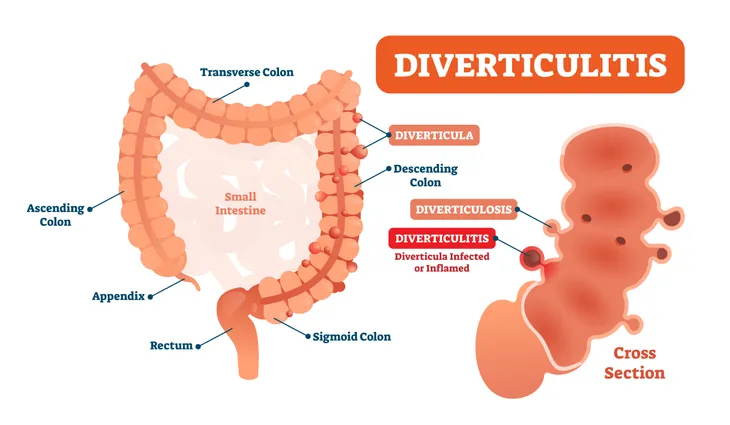
1. Diverticulitis
Diverticulitis is the most common cause of LLQ pain. It represents inflammation and infection of one or more diverticula, small pouches in the large intestine (colon). Diverticula represent weak spots in the wall of the large intestine. Most diverticula occur in the sigmoid colon. Diverticulosis, or the abnormal development of diverticula in the colon, is a common condition in middle aged and older adults. As a result, diverticulitis is generally considered a disease of the elderly.
Accompanying signs and symptoms may include nausea and vomiting, constipation, diarrhea, bloating, flatulence (excessive gas), or fever. Computed tomography (CT) scanning of the abdomen is considered the best imaging study to confirm the diagnosis. Treatment of diverticulitis includes being made NPO (nothing by mouth), antibiotic therapy, and advancing the diet as tolerated. Complications of diverticulitis may include fistulas (abnormal connections between organs), abscess, intestinal obstruction, peritonitis, and sepsis (an overwhelming response to a life-threatening infection).
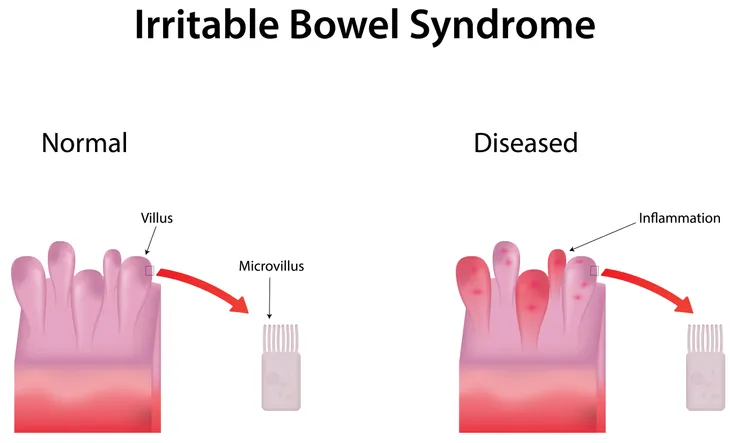
2. Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is a chronic gastrointestinal (GI) disorder. IBS is a diagnosis of exclusion, which means a diagnosis of a medical condition reached by a process of elimination. Typically, potentially life-threatening conditions are the first to be eliminated. The cause of IBS is unknown, but is thought to result from a combination of abnormal GI tract movements; miscommunication between the brain and GI tract; and increased awareness of bodily functions.
Symptoms of IBS may include abdominal pain or cramping, bloating, gas, and altered bowel habits (e.g. diarrhea or constipation). These symptoms should be present at least three months. Despite extensive investigation (e.g. blood studies, imaging studies, stool examinations, and colonoscopy), no organic disease is identified. Four bowel patterns may be seen with IBS—diarrhea predominant (IBS-D), constipation predominant (IBS-C), mixed diarrhea and constipation (IBS-M), and unclassified (IBS-U). Treatment primarily consists of dietary avoidance and psychological support.
3. Lactose Intolerance
Lactose intolerance is a common disorder and is characterized by a deficiency of the enzyme lactase, which helps digest lactose into glucose and galactose. Both glucose and galactose are simple sugars. Elevated blood lactose levels are responsible for the symptoms of lactose intolerance. Lactose is present in dairy products such as milk, butter, cheese, and ice cream. The disorder is more likely to affect those of Asian, African, or Native American descent.
Symptoms of lactose intolerance may include loose stools, abdominal pain, bloating, flatulence (excessive gas), borborygmi (stomach rumble), and nausea. Dietary adjustment (reduce or restrict eating foods containing lactose) is the primary form of treatment for lactose intolerance. Lactose intolerance is not life threatening. Complications of lactose intolerance may include osteopenia (bone density that is lower than normal, but not low enough to be classified as osteoporosis). As a result, calcium supplementation is recommended for individuals who are lactose intolerant.
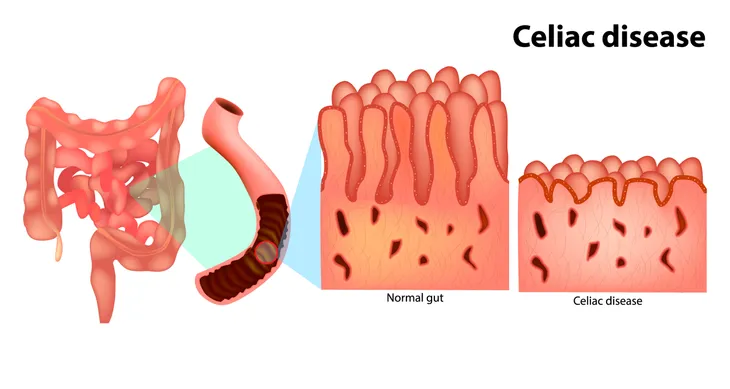
4. Celiac Disease
Celiac disease, also known as celiac sprue or gluten-sensitive enteropathy, is a chronic disorder of the digestive tract. It represents an inability to tolerate gluten, a protein commonly found in wheat, rye, and barley. Microscopically, the immune system attacks the mucosa of the intestines resulting in maldigestion and malabsorption. The frequency of celiac disease in the U.S. is relatively low (about one case in every 133 individuals).
Symptoms of celiac disease may include abdominal pain, diarrhea, flatulence (excessive gas), weight loss, borborygmi (stomach rumble), and fatigue. The primary treatment of celiac disease is dietary—avoidance of gluten. Corticosteroids such as prednisone may have to be used in individuals with progression of celiac disease despite dietary adjustment. Corticosteroids have anti-inflammatory properties, as well as modify the body’s immune response to the mucosa of the intestines. The prognosis for individuals (correctly diagnosed and treated) is excellent.
5. Kidney Stones
Kidney stones, also referred to as nephrolithiasis, are a common disorder of the urinary tract. Dilation, stretching, and spasm of the urinary tract cause the pain associated with kidney stones. The condition is ancient and has been found in Egyptian mummies. The majority of kidney stones consist of calcium. Uric acid comprises the bulk of the minority of kidney stones. Other less frequent kidney stone types include cystine and struvite (magnesium ammonium phosphate).
Symptoms of kidney stones may include flank and/or lower abdominal pain, dysuria (painful urination), hematuria (blood in the urine), nausea and vomiting, urinary frequency, or fever and chills. Computed tomography (CT) scanning of the abdomen is the primary imaging study used to diagnose kidney stones. Approximately 80 to 90-percent of kidney stones pass spontaneously. Analysis of passed kidney stones will reveal their composition and may be helpful in the treatment of recurring stones.
6. Constipation
Constipation is the most common digestive complaint in the US. Signs and symptoms of chronic constipation may include:
- Fewer than three bowel movements per week
- Straining
- Lumpy or hard stools
- Sensation of a blockage in the anus or rectum
- Sensation of not completely emptying rectum
- Manual maneuvering, such as applying pressure to the abdomen with hands or using a finger to remove stool, is required to have a bowel movement
Treatment of chronic constipation is primarily diet and lifestyle adjustments. Regular exercise, gradual increase in fiber intake, increased water intake, and paying attention to the urge to defecate are all recommended. Fiber is arguably the best and least expensive medication for constipation. The use of polyethylene glycol (MiralaxTM) is increasing as first-line therapy for chronic constipation. Complications of constipation may include hemorrhoids, anal fissures, fecal impaction, and rectal prolapse.
7. Crohn’s Disease
Crohn’s disease is a characterized by chronic inflammation that may affect any part of digestive tract from the mouth to the anus. It is one of two major types of inflammatory bowel disease. Most commonly it affects the small intestine or the large intestine (colon). The exact cause of Crohn disease is unknown. The age of onset of the disease has two peaks—one between ages 15 and 30-years and a second between ages 60 and 70-years.
Abdominal pain and diarrhea are the most common presenting symptoms of Crohn disease. Other symptoms may include rectal bleeding, fever, weight loss, fatigue, nausea, vomiting, and bone loss. Imaging studies and colonoscopy with biopsy are crucial to the diagnosis of Crohn disease. Corticosteroids, 5-aminosalicylic acid derivatives, and immunosuppressive agents are the primary drugs used to treat Crohn disease. Surgical management is not a cure, but may be necessary for refractory, or hard to treat, cases.
8. Ulcerative Colitis
Ulcerative colitis is a chronic inflammatory condition of the colon. It is the second of two major types of inflammatory bowel disease. Ulcerative colitis typically only affects the large intestine, or colon. The exact cause of ulcerative colitis is unknown. It occurs more frequently in whites compared to African Americans or Hispanics. Ashkenazi Jews have the highest risk of developing ulcerative colitis.
Symptoms of ulcerative colitis may include abdominal pain and cramping, diarrhea, rectal bleeding, weight loss, fever, and fatigue. The disease is best diagnosed with colonoscopy and biopsy. Corticosteroids, 5-Aminosalicylic acid derivatives, and immunosuppressive agents are the primary drugs used to treat ulcerative colitis. The most common cause of death amongst patients with ulcerative colitis is toxic megacolon (the term for acute toxic colitis with dilation, or widening, of the colon). The disease also increases the risk of developing colon cancer.
9. Intestinal Obstruction
Intestinal obstruction is a blockage that prevents food from passing through the small intestine or large intestine (colon) and is an emergency condition. Its frequency increases with age. As a result, intestinal obstruction is more common in the elderly. The most common causes of colonic obstruction are colon cancer, diverticulitis, and intestinal adhesions (scar tissue forming between opposing surfaces after surgery or infection).
Symptoms of colonic obstruction may include abdominal pain, constipation, abdominal distention, nausea and vomiting, and inability to have a bowel movement or pass gas. Computed tomography (CT) scanning of the abdomen is the imaging modality of choice for the diagnosis of colonic obstruction. Treatment typically requires hospitalization. Complications of intestinal obstruction may include the death of intestines and peritonitis (infection of the abdominal cavity), which are both considered serious and life threatening.
10. Inguinal Hernia
An inguinal, or groin, hernia occurs when the intestines protrude through a weak spot in the abdominal muscles. It is a type of abdominal wall hernia, which are probably the most common of all surgical problems. Inguinal hernias (75-percent) are the most common of the abdominal wall hernias. They may be classified as either direct or indirect, with the majority being indirect. Inguinal hernias affect men much more often than women. The majority of inguinal hernias occur on the right side.
Signs and symptoms of an inguinal hernia may include a bulge in the groin area, a burning or aching sensation at the bulge, pain in the groin, and a heavy or dragging sensation in the groin. The bulge may be more obvious sitting upright or with coughing or straining. A physical examination is all that is needed to diagnose an inguinal hernia. Most inguinal hernias require surgical repair. Complications of inguinal hernias may be incarcerated hernia and bowel strangulation.
11. Shingles
Shingles, also known as herpes zoster, is a viral infection causing a painful rash. The rash usually appears as a single stripe of blisters wrapping around the left or right torso and never crossing the midline of the body. Shingles is caused by the reactivation of the varicella-zoster, or chickenpox, virus (which is typically acquired as a kid). After the resolution of the chickenpox, the virus may lay dormant in the nerve roots for decades.
Shingles is primarily a disease of adults. It can be divided into three phases: pre eruptive stage, acute eruptive stage, and chronic phase (postherpetic neuralgia). Oral antiviral drugs (acyclovir, famciclovir, and valacyclovir) may be beneficial, but are most effective if initiated within 72-hours of symptom onset. Vaccines are available for the prevention of shingles. Complications of shingles may include postherpetic neuralgia (persistent or recurring nerve pain lasting 30 or more days after acute infection).
12. Pseudomembranous Colitis
Pseudomembranous colitis is inflammation of the colon caused by an infection with the bacterium Clostridium difficile. The release of bacterial toxins causes inflammation and damage to the colon. The disease most commonly affects the elderly in hospitals or nursing homes and typically occurs after treatment with antibiotic medications. The antibiotics most closely associated with causing the disease include fluoroquinolones, cephalosporins, penicillins, and clindamycin.
Symptoms of pseudomembranous colitis may include watery diarrhea with abdominal cramping and tenderness. It is not uncommon to see blood or pus in the stool. The disease is diagnosed using stool tests that detect toxins produced by C. difficile. Ironically, the treatment for pseudomembranous colitis is another antibiotic, metronidazole (FlagylTM). Complications of pseudomembranous colitis may include dehydration, kidney failure, bowel perforation (rupture), toxic megacolon, and death. Recurrence of infection occurs in up to 20-percent of individuals diagnosed with pseudomembranous colitis.