Travel medicine is a multidisciplinary field concentrating on prevention of infectious diseases and patient safety during international travel. Advising international travelers on vaccine-preventable diseases is increasingly becoming the responsibility of primary care physicians (PCPs). Physicians should maintain familiarity with current recommendations for travel health safety. Today, international travel to exotic locales is commonplace. Travel vaccines generally fall into one of three categories—childhood immunizations that should be updated or boosted, legally required immunizations necessary for entry into certain countries, and recommended immunizations that depend on the risks of exposure at the travel destination.
Ten vaccinations for international travelers are…
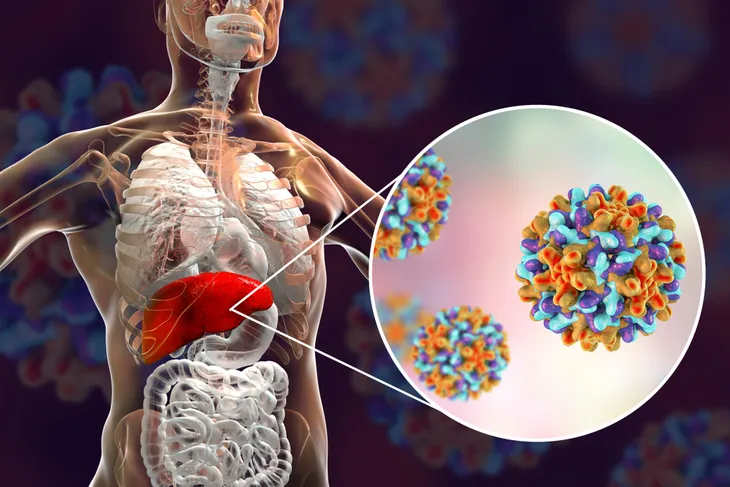
1. Hepatitis A
Hepatitis represents inflammation of the liver. Hepatitis A is an acute infectious disease of the liver caused by the hepatitis A virus (HAV). The disease is transmitted through ingestion of contaminated food and water or through direct contact with an infectious person. Almost everyone recovers fully from hepatitis A. Improved sanitation and the hepatitis A vaccine are the most effective ways to combat the disease.
The Infectious Diseases Society of America (IDSA) recommends the hepatitis A vaccine for the following groups—travelers to developing countries; children 12-months and older; persons with clotting disorders or chronic liver disease; and anyone engaging in risky sex behavior. The hepatitis A vaccine is administered as 2-shots, at least 6 to 12-months apart. Preferably, the first dose of vaccine should be provided 4-weeks prior to departure. The vaccine provides protective antibody levels in 94 to 100-percent of patients within 4-weeks of vaccination. Common adverse effects of this vaccine include injection site soreness and headaches.
2. Hepatitis B
Hepatitis refers to inflammation of the liver. Hepatitis B is caused by the hepatitis B virus (HBV), which can cause acute and chronic disease. The virus is transmitted through contact with the blood or other body fluids of an infected person. Hepatitis B is an important occupational hazard for healthcare workers. It can be prevented with the safe and effective hepatitis B vaccine.
Despite childhood vaccination against hepatitis B being routine in the United States, many adult travelers have not been immunized. The hepatitis B vaccine is recommended for the following groups—healthcare workers who come in contact with blood; persons at risk of coming in contact with blood, body fluids, or blood-contaminated medical or dental instruments; and persons residing or traveling in areas of intermediate to high risk for hepatitis B (South America, Africa, southeast Asia, and South Pacific). The standard schedule for vaccinations is a series of 3-injections at 0, 1, and 6-months. Common adverse effects of this vaccine include injection site soreness and headaches.
3. Poliomyelitis
Poliomyelitis, also known as polio, is a highly contagious viral disease that can cause paralysis, dyspnea (difficulty breathing), and occasionally death. In the United States, the last case of naturally occurring polio was documented in 1979. Today, despite global eradication programs, polio still affects children and adults in different parts of the world. The virus is transmitted mainly by person-to-person spread and less commonly through contaminated water or food. It is easily preventable with the administration of the polio vaccine.
The United States Centers for Disease Control and Prevention (CDC) advises measures to protect against contracting polio if traveling to an area with high risk (India, Nigeria, Pakistan, Egypt, Afghanistan, Niger, and Somalia). Previously vaccinated adults planning to travel to an area of high risk should receive a booster dose of inactivated polio vaccine (IPV). Immunity after a booster dose of IPV lasts a lifetime. Common adverse effects of this vaccine include injection site soreness, low-grade fever, and joint pain.
4. Influenza
Influenza, or flu, is an acute viral infection caused by the influenza virus. There are three types of influenza virus—A, B, and C. These viruses are found in all parts of the world. Type C influenza virus cases occur much less frequently than A and B. As a result, only influenza A and B viruses are included in influenza vaccines. Influenza viruses can cause annual epidemics that peak during the winter months in temperate, or mild, climates. At times, influenza can present a serious public health problem.
Vaccination for influenza is the most effective way to prevent infection. Annual vaccination is recommended in all persons 6-months and older. During a vaccine shortage, the flu vaccine is a priority for the following groups: children 6-months to 4-years; persons with chronic diseases; healthy adults 50-years and older; pregnant women; health care workers; and residents of nursing homes. The flu vaccine is available by injection or nasal spray.
5. Japanese Encephalitis
Japanese encephalitis is the most common cause of viral encephalitis in Asia. The causative virus is transmitted through the bite of mosquitoes. The disease is prevalent in the Indian subcontinent, China, Korea, Japan, and other countries in Southeast Asia. Most individuals infected with Japanese encephalitis have no symptoms, but according to the World Health Organization (WHO) severe cases can result in a death rate as high as 30-percent. Furthermore, permanent neurologic and psychiatric complications can occur in 30 to 50-pecent of individuals diagnosed with encephalitis.
Encephalitis refers to inflammation of the brain. The Japanese encephalitis (JE) vaccine should be offered to individuals who plan to remain for 30-days or longer in areas of prevalent transmission of the disease. Primary immunization against JE consists of a series of 3-injections at days 0, 7, and 30. A booster injection is needed every 2 to 3-years. Adverse effects of the JE vaccine include fever, headache, nausea, and vomiting.
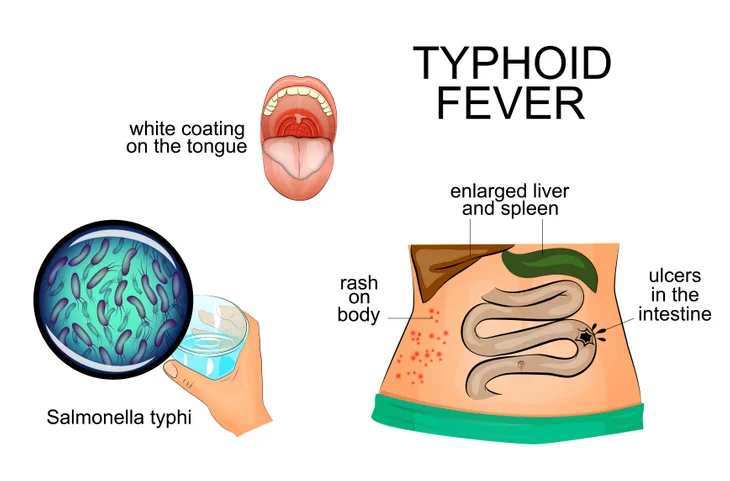
6. Typhoid Fever
Typhoid fever is a bacterial disease caused by the bacteria Salmonella typhi. The disease is transmitted through contaminated food and water. Symptoms usually develop 1 to 3-weks after initial exposure and may include high fever, headache, constipation or diarrhea, and enlarged spleen and liver. It can be treated with antibiotics. However, resistance to common antibiotics used to treat the disease is widespread.
Typhoid fever vaccine is recommended for travelers visiting areas where the disease is prevalent, which includes Central and South America, the Indian subcontinent, and Africa. There are two typhoid vaccines, one oral and one injectable, currently available on the market. Primary vaccination with the oral vaccine, Ty21a, consists of 1-capsule taken every other day for a total of 4-capsules. Primary vaccination with the injectable vaccine, Typhim VI, consists of a one-time intramuscular injection. Boosters can be given every 5-years for Ty21a and every 2-years for Typhim VI. Adverse effects may include nausea, vomiting, cramping, and fever.
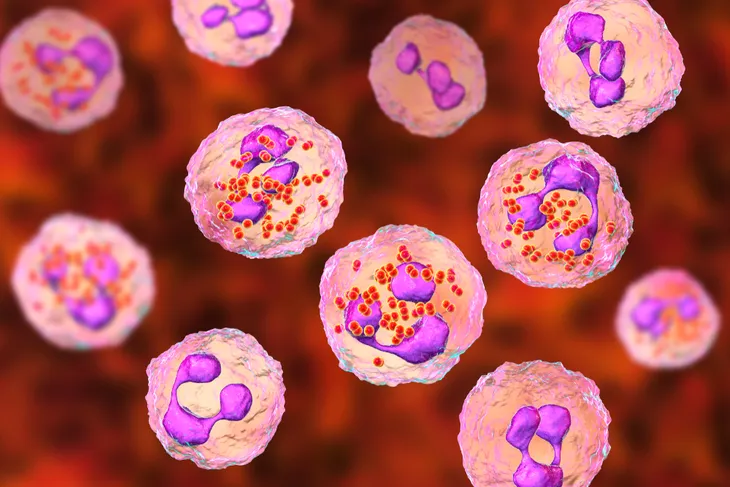
7. Meningococcal
Meningococcal meningitis is a bacterial form of meningitis caused by the bacteria Neisseria meningitides. Meningitis refers to inflammation of the meninges, which are composed of three membranes covering the brain and spinal cord. Meningococcal meningitis can cause severe brain damage and leads to death in 50-percent of cases if untreated. Symptoms of meningitis may include high fever, severe headache, stiff neck, nausea, vomiting, decreased appetite, sensitivity to light, and skin rash.
Meningococcal vaccine (Menomune) is recommended for travelers to sub-Saharan Africa. The area known as the “meningitis belt” stretches from Senegal to Ethiopia. The vaccine is required for religious pilgrims to Saudi Arabia. Researchers report protective levels of antibodies in 7 to 10-days after vaccination. Primary vaccination is with a single subcutaneous injection. Booster doses should be given every 3 to 5-years for continued travel or exposure. The most common adverse effect of administration of the meningococcal vaccine is injection site soreness.
8. Rabies
Rabies is a viral disease transmitted to humans from domestic and wild animals. The organism is present in saliva and is spread via bites or scratches. There are high rates of canine rabies in areas such as the Indian subcontinent, China, Southeast Asia, the Philippines, parts of Indonesia, Latin America, Africa, and countries of the former Soviet Union.
Dog bites are the source of the vast majority of human rabies deaths. According to the World Health Organization (WHO), more than 95-percent of human deaths attributed to rabies occur in Asia and Africa. The rabies vaccine should be offered to individuals anticipating a stay greater than 30-days in areas with high rates of rabies, work near animals, engage in activities that could attract animals, or who cannot report an exposure if bitten. Primary vaccination for rabies consists of a series of three intramuscular injections on days 0, 7, and 21 or 28.
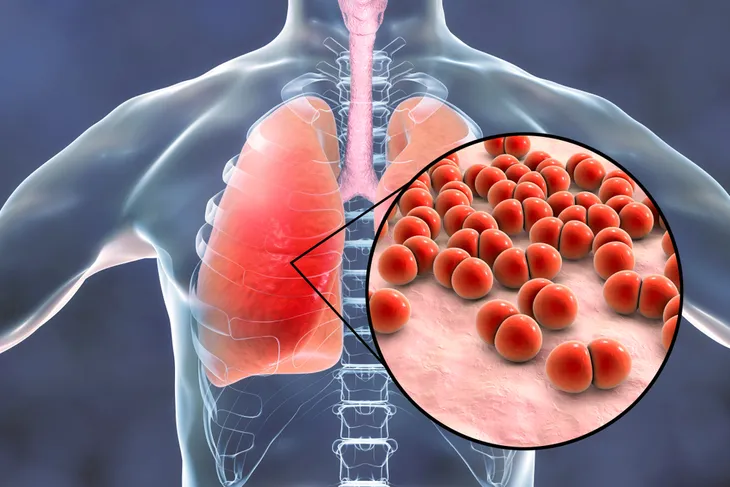
9. Pneumococcal
Streptococcus pneumoniae is a bacterium that causes a number of common diseases term pneumococcal diseases. The bacterium can cause a variety of diseases including meningitis (infection of membrane surrounding brain and spinal cord), septicemia (blood infection), pneumonia (lung infection), sinusitis (sinus infection), and otitis media (middle ear infection). Rates of disease and death from pneumococcal disease are higher in developing countries compared to industrialized countries, with the majority of deaths occurring in sub-Saharan Africa and Asia.
Pneumococcal diseases are most common in young children and the elderly. There are currently two types of pneumococcal vaccines: PCV13 (Prevnar) and PPSV23 (Pneumovax). Prevnar is recommended for all children younger than 5-years, all adults 65-years or older, and individuals 6-years and older at high risk. Pneumovax is recommended for all adults who are 65-years or older and individuals 2 to 64-years old at high risk. The use of pneumococcal vaccines has dramatically reduced the incidence of pneumococcal disease.
10. Yellow Fever
Yellow fever is rare but potentially fatal viral disease that most commonly occurs in equatorial Africa and South America. The virus that causes the disease is transmitted through the bite of mosquitoes. Yellow fever symptoms vary and may include fever, hepatitis (inflammation of the liver), jaundice (yellow skin or eyes), kidney failure, vomiting blood, shock, and death. Individuals with yellow fever usually have to be hospitalized.
Yellow fever vaccine can prevent yellow fever. Yellow fever vaccination is recommended for individuals older than 9-months who are traveling to areas where yellow fever is reported. Many countries where yellow fever is common require vaccination for entry. Primary vaccination is achieved with a single subcutaneous injection of the vaccine. Vaccination produces neutralizing antibodies in 99-percent of patients within 30-days of receipt. Immunity is likely lifelong, but a booster vaccination is recommended every 10-years. Adverse effects reported with yellow fever vaccination include headaches, fever, and myalgias (muscle pain).