November is Prostate Cancer Awareness Month and men should consider getting screened for prostate cancer with a digital rectal examination (DRE) and prostate specific antigen (PSA) blood test. The DRE Involves a physician inserting a gloved, lubricated finger into the rectum to palpate, or feel, any abnormalities in the prostate. The American Cancer Society (ACS) recommends men commence prostate cancer screening at age 50, while men at high risk (African-American, positive family history) should be considered at age 40 or 45. According to the ACS, prostate cancer is the most common non skin cancer among men in the United States. It occurs mostly among men aged 65 or older (60-percent).
Ten treatments for prostate cancer are…
1. Watchful Waiting
Watchful waiting, also referred to as observation, is based on the premise that some men will not benefit from aggressive treatment of their prostate cancer. The treatment option is usually agreed upon shortly after the diagnosis of prostate cancer. Men with prostate cancer who choose this option for treatment will undergo less intensive follow-up of their cancer. It usually translates into fewer physician visits and tests such as DREss, PSAs, MRI or CT scans, and prostate ultrasounds with or without biopsies.
Men choosing watchful waiting usually have clinically localized, or low-risk, disease and a life expectancy of less than 10-years. In other words, the prostate cancer is confined within the prostate and these men will probably die from other diseases before prostate cancer. The majority of prostate cancers grow slowly. Men undergoing watchful waiting forego curative treatment, but may receive treatment for bothersome symptoms related to the advancement or spread (metastasis) of prostate cancer.
2. Active Surveillance
Active surveillance is based on the premise that some men will benefit from treatment of their prostate cancer. After the diagnosis of prostate cancer, men choosing this treatment option will undergo examinations and tests at regular intervals (usually no often than every 6 to 12-months unless clinically indicated). Active surveillance may be recommended if a man’s prostate cancer is causing no symptoms, is expected to grow slowly, and/or is contained within the prostate. Treatment, which is usually curative, may be initiated if the prostate cancer is growing or advancing.
Active surveillance of prostate cancer has two goals: to provide potentially curative treatment for men with localized cancers likely to advance and to reduce the risk of treatment related complications for men with cancers that are not likely to advance. Treatment may be initiated based on rising PSA levels or a change in the DRE, ultrasound results, or biopsy findings. Treatment most commonly involves surgery or radiation therapy.
3. Radical Prostatectomy
Radical prostatectomy is a surgical procedure involving the complete removal of the prostate, surrounding tissue, and several lymph nodes. It is often curative if the prostate cancer has not spread outside the prostate. A radical prostatectomy can be performed using various techniques. The open approach involves removing the prostate and nearby tissues through a single long incision and is used less frequently nowadays. The open approach can be retropubic (incision is made in the abdomen and prostate is removed from behind the pubic bone) or perineal (incision is made in the space between the scrotum and the anus).
More often today, the radical prostatectomy approach is laparoscopic (surgery is performed through several small incisions in the abdomen with special instruments). In an even newer approach, the laparoscopic radical prostatectomy is performed using robotic assistance called the da Vinci system. The surgery can also be nerve-sparing (preserves erectile function) or non-nerve-sparing. The most common adverse effects of radical prostatectomy are urinary incontinence and erectile dysfunction.
4. Radiation Therapy
Radiation therapy uses high-energy particles (photons and X-rays) to kill cancer cells. Prostate cancer radiation therapy can be administered in two ways: external beam radiation therapy (EBRT) and brachytherapy (internal radiation therapy). In EBRT, beams of radiation are focused on the prostate from a machine outside the body. It can be used as a curative treatment in localized prostate cancer or for symptomatic treatment of pain associated with the spread (metastasis) of prostate cancer. The treatment is usually 5-days a week for a total of approximately 7 to 9-weeks.
Brachytherapy (internal radiation therapy) is also known as seed implantation. During this therapy, small radioactive pellets (“seeds”) are placed directly into the diseased prostate. Ultrasound, MRI, or CT scan may guide placement of the radioactive pellets. Brachytherapy is an acceptable choice for men whose cancer is confined within the prostate. Possible adverse effects of radiation therapy may include frequent urination, rectal pain, diarrhea, and erectile dysfunction.
5. Hormone Therapy
Hormone therapy is also called androgen deprivation therapy (ADT), which is a technique used to stop the production of male hormones called androgens. The main androgens are testosterone and dihydrotestosterone. Androgens, mainly testosterone, fuel the growth of prostate cancer cells. Hormone therapy treatment options for prostate cancer include medications that lower androgen levels or prevent androgens from working on cancer cells. Orchiectomy, or surgical removal of the testicles, also reduces levels of androgens in the body.
Hormone therapy is an excellent choice in men with advanced prostate cancer as it helps shrink and slow the growth of tumors. Many times curative treatment with surgery or radiation is not possible or acceptable in this group. Adverse effects of ADT may include hot flashes, decreased sex drive, loss of bone mass, weight gain, and erectile dysfunction.
6. Chemotherapy
Chemotherapy uses powerful drugs to kill prostate cancer cells. The drugs are injected into a vein (intravenous) or taken by mouth in pill form. Chemotherapy drugs work by entering the bloodstream and stopping the division of cancer cells, which stops the growth and spread of cancerous tumors. Chemotherapy is usually administered in cycles and each treatment period is followed by a period of rest in order to allow recovery.
Chemotherapy is not used for cancer confined within the prostate. It is a treatment option for men with prostate cancer that has spread to distant areas of the body (metastasized) or for those who do not respond to treatment with hormone therapy. Chemotherapy is very unlikely to cure prostate cancer. It can exact a toll on the body and common adverse effects may include hair loss, mouth sores, nausea, vomiting, diarrhea, loss of appetite, fatigue, easy bruising or bleeding, and increased chances of developing infections.
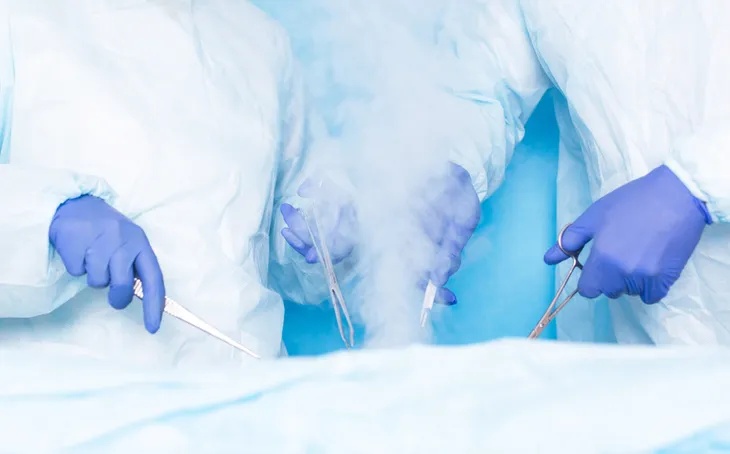
7. Cryosurgery
Cryosurgery, also called cryotherapy or cryoablation, is a procedure that uses extremely cold temperatures to freeze and destroy prostate cancer cells. During this procedure, a physician uses ultrasound guidance to place several hollow needles into the prostate. A freezing liquid (nitrogen or argon gas) is introduced into the prostate through the needles. The intensely cold temperatures destroy any cancerous cells within the prostate.
Cryosurgery is usually not used as an initial treatment for prostate cancer. It may be an option for men who are in the early stages of prostate cancer or who have not responded to treatment with radiation therapy. Cryosurgery is less invasive than radical prostatectomy and other advantages include less blood loss, shorter hospital stay, shorter recovery period, and less swelling and pain. Possible adverse effects of cryosurgery include blood in the urine (hematuria), swelling of the penis or scrotum, urinary frequency, urinary incontinence, and erectile dysfunction.
8. Vaccine Therapy
Vaccine therapy, also known as biological therapy or immunotherapy, uses the immune system to kill prostate cancer cells. White blood cells, which help us fight infection and are major components of the immune system, are removed from the patient while he is hooked up to a special machine. The white blood cells are then sent to a lab and exposed to proteins on prostate cancer cells. The same cells are given back to the patient via infusion into a vein (intravenous).
The vaccine is custom made for each individual patient seeking treatment for prostate cancer. A usual course of treatment is 3-doses with each being 2-weeks apart. The vaccine is not curative and is usually reserved for treating advanced prostate cancer that has failed hormone therapy. Common adverse effects of the vaccine may include fever, chills, fatigue, nausea, headache, and back or joint pain. The adverse effects are usually transient and last no longer than a few days.
9. Bisphosphonate Therapy
Bisphosphonates are a class of drug that prevent the loss of bone mass. Bone is the most common area of spread, or metastases, for prostate cancer. A study from Washington University School of Medicine estimates bone metastases occur in 80-percent of men with advanced prostate cancer. When prostate cancer spreads to bone, it may cause complications such as pain, compression of the spinal cord, and fractures. Bisphosphonate therapy may help prevent these complications.
Bisphosphonate therapy works by inhibiting osteoclasts (cells that break down bone). The therapy is most commonly injected into a vein (intravenous) once every 3 to 4-weeks. Patients also are advised to take supplements of calcium and vitamin D. The most common adverse effects of bisphosphonate therapy are flu-like symptoms and joint or bone pain. A rare but very serious adverse effect of bisphosphonates is osteonecrosis of the jaw (bone loses its blood supply and dies).
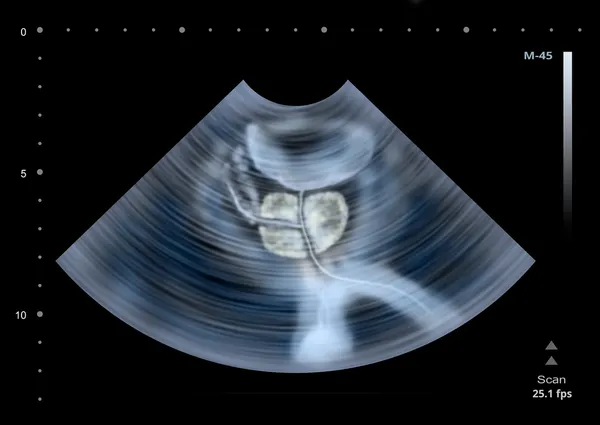
10. High-Intensity Focused Ultrasound
High-intensity focused ultrasound (HIFU) is an emerging treatment for prostate cancer. Instead of using extremely cold temperatures as in cryosurgery, HIFU utilizes heat to destroy cancer cells. The heat is in the form of very high-intensity ultrasound waves. During the procedure, a physician inserts a probe into the rectum and delivers very high-intensity ultrasound waves to the target area in the prostate. These waves heat up the tissue and kill prostate cancer cells.
In the United States, HIFU is experimental and is not approved by the Food and Drug Administration (FDA) for the treatment of prostate cancer. The procedure has been available since 1993 in Europe, Canada, and Mexico. It may be useful in men who have failed radiation therapy or who have had recurrences of cancer after surgery to remove the prostate. The most common adverse effects of treatment with HIFU are urinary incontinence, urinary tract infection, and erectile dysfunction.