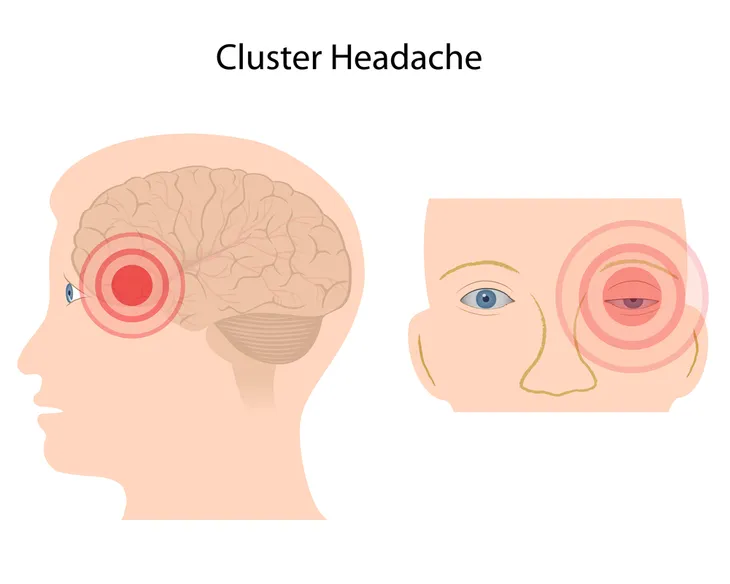
Cluster headaches occur in a cyclical pattern, or cluster, which can last fifteen to 180-minutes for weeks to months. They are the most severe of headaches and are referred to by some as “suicide headaches.” The exact cause of cluster headaches is unknown. They are more common in men and typically start before age 30. A study from Germany estimates 1 in 1,000 adults experience cluster headaches. Symptoms include intense pain in or around an eye with associated redness, excessive tearing, swelling, constriction of pupil, eyelid drooping, and nasal discharge or congestion.
Ten treatments for cluster headaches are…
1. Oxygen
Oxygen is a first-line agent in the acute treatment of cluster headaches. It is considered an abortive medication, which is intended to stop cluster headaches from progressing any further. In a trial published in the Journal of the American Medical Association, inhaled oxygen (100-percent) at 12-liters/minute was more effective than placebo in eliminating pain after 15-minutes of administration (78-percent vs. 20-percent).
An Australian trial suggested that hyperbaric oxygen (administered at environmental pressures greater than 1-atmosphere) was more effective than normobaric oxygen (administered at 1-atmosphere) at aborting cluster headaches.
There are no reported adverse effects when administering oxygen in the acute treatment of cluster headaches. The administration of hyperbaric oxygen has two significant drawbacks—cost and lack of accessibility. The cost of administration of normobaric oxygen is cheap, but this method of treatment suffers from inconvenience and lack of accessibility. No evidence exists indicating oxygen prevents future cluster headaches.
2. Triptans
Triptans are also first-line agents in the acute treatment of cluster headaches. Like oxygen, they are also abortive agents. Triptans were first used as agents for the treatment of migraine headaches. A study from the University of Oxford in England found a 6-mg subcutaneous dose of sumatriptan (Imitrex) was more effective than placebo at relieving pain 15-minutes after injection (75-percent vs. 32-percent). In the same study, a 10-mg intranasal dose of zolmitriptan (Zomig) was also better than placebo at relieving pain 30-minutes after administration (62-percent vs. 26-percent).
Adverse effects reported with the injection of sumatriptan include dizziness, fatigue, nausea, vomiting, injection site reactions, and paresthesias (sensation of pins and needles on skin). Adverse effects reported with the intranasal administration of zolmitriptan (Zomig) included bad taste, nasal cavity discomfort, and somnolence (drowsiness). Individuals with coronary artery disease or uncontrolled high blood pressure (hypertension) should not receive triptans.
3. Lidocaine
Lidocaine (Xylocaine) is a local anesthetic, which causes the reversible loss of sensation during surgical procedures. Other uses in medicine include treatment of nerve pain (neuropathy), ringing in the ears (tinnitus), abnormal heart rhythms (arrhythmias), and cough (antitussive).
In a trial at the Robbins Headache Clinic in Illinois, 30 male patients received intranasal administration of 4-percent lidocaine (4 sprays in the nostril on the affected side) as an abortive treatment for acute cluster headaches. It was found to be only marginally effective for the treatment of acute cluster headaches, as 46-percent of patients reported no relief from lidocaine. Adverse effects of intranasal lidocaine included nasal congestion and unpleasant taste. Due to its ease of administration and lack of adverse effects, it may be worthwhile to further study lidocaine as an adjunct, or add-on, to other treatments of acute cluster headaches such as oxygen and triptans.
4. Octreotide
Octreotide (Sandostatin) mimics the naturally occurring hormone somatostatin, which is also known as growth hormone-inhibiting hormone. Octreotide is used for the treatment of acromegaly (gigantism), VIPomas, and carcinoid tumors. A VIPoma is a tumor involving the cells that produce vasoactive intestinal peptide (VIP) in the pancreas. Carcinoid tumors are primarily found in the gastrointestinal tract and may lead to carcinoid syndrome, which is characterized by flushing of the skin and diarrhea. Off-label uses (not approved by the U. S. Food and Drug Administration) include the treatment of bleeding esophageal varices (enlarged veins) and dumping syndrome.
In a study from London, subcutaneous injection of octreotide in a dose of 100-micrograms was significantly superior to placebo in the acute treatment of cluster headaches (52-percent vs. 36-percent) 30-minutes after administration. Adverse effects of octreotide include bloating, diarrhea, constipation, vomiting, background headaches, dizziness, injection site reactions, nausea, and lack of energy (lethargy).
5. Ergots
Ergotamine and dihydroergotamine (DHE) belong to the group of medications known as ergots. Ergots can be used to treat migraine headaches. They also can be used to treat and prevent acute cluster headaches. Ergotamine causes the blood vessels in the body to narrow (vasoconstrict). It can be used under the tongue (sublingually) for the prevention of cluster headaches. Dihydroergotamine is a derivative of ergotamine. Self-injected DHE may be helpful in preventing acute cluster headaches, while intravenous DHE has been shown to effectively treat acute cluster headaches.
A study published in Headache found that repetitive intravenous dihydroergotamine safely, rapidly, and effectively controls cluster headache. All 54 patients enrolled in the study had complete relief of their cluster headaches, usually within 2-days. Adverse effects of the ergot class include chest pain (angina), myocardial infarction (heart attack), scarring (fibrosis), itching (pruritis), and dizziness (vertigo).
6. Verapamil
Verapamil belongs to the class of medications called calcium channel blockers, which are primarily used to treat high blood pressure (hypertension). It is the medication of first resort for the prophylaxis, or prevention, of cluster headaches. Verapamil is sold under the brand names Calan and Verelan. It is used in a minimum oral dosage of 240-mg in a single or divided dose per day. A Canadian study published in Neurology reported a 50-percent reduction in chronic cluster headaches treated with verapamil. It can take 2- to 3-weeks for the full effect of this medication.
Adverse effects reported with verapamil include slow heart rate (bradycardia), constipation, low blood pressure (hypotension), and enlargement of the gums (gingival hyperplasia). Patients using this medication will also need periodic heart tracings (electrocardiograms) to monitor for heart block. In individuals with heart block, the electrical signals controlling the heart are partially or completely blocked from reaching the lower chambers of the heart (ventricles).
7. Lithium
Lithium (Eskalith) is a mood stabilizing medication, which is primarily used to treat bipolar disorder (manic depression). Like verapamil, it is used for the prophylaxis, or prevention, of cluster headaches. A Canadian study published in Neurology reported a 37-percent reduction in chronic cluster headaches treated with lithium. The benefits of this medication usually appear within 2-weeks of starting the drug.
An oral dosage of 800- to 900-mg with meals in divided doses is recommended. Adverse effects of lithium include trembling hands (tremors), nausea, increased thirst, excessive urination (polyuria), and hypothyroidism (low functioning thyroid gland). Blood levels of lithium should be monitored every 6-months and with changes in dose to guard against toxicity. Kidney and thyroid gland function also need to be monitored periodically while on this medication.
8. Corticosteroids
Oral corticosteroids (steroids) are potent inhibitors of inflammation and can be used in the prevention of chronic cluster headaches. They appear to be most useful as bridging therapy until another prophylactic medication such as verapamil or lithium becomes therapeutic. Prednisone is the prototypical corticosteroid. It is typically taken orally in a dose of 50 to 80-mg per day, which is gradually tapered over 10- to 12-days.
Long-term use of corticosteroids is not recommended due to the potential for serious adverse effects such as elevated blood sugar (hyperglycemia), high blood pressure (hypertension), increased appetite, insomnia, and nervousness. No adequate clinical trials exist that find corticosteroids useful in the long-term treatment of chronic cluster headaches.
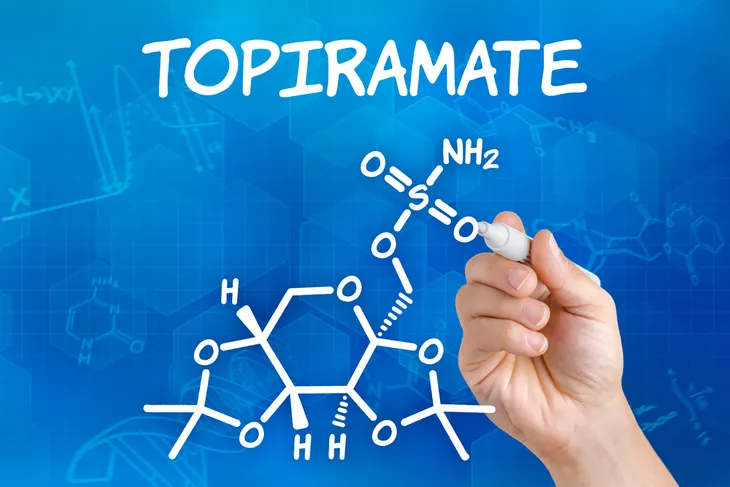
9. Topiramate
Topiramate (Topamax) is an anti-seizure used in the treatment of epilepsy. In several small studies, it has been shown to be effective for the prophylaxis, or prevention, of chronic cluster headaches. The exact mechanism of action in the setting of cluster headaches is unknown. A study from Spain published in Headache reported the remission of chronic cluster headaches in 60-percent of patients treated with topiramate. These patients were treated with very low doses (25- to 75-mg per day).
Adverse effects seen with topiramate include dizziness, fatigue, nervousness, paresthesias (sensation of tingling, tickling, pricking, or burning of the skin), hair loss (alopecia), and loss of appetite (anorexia). It should not be prescribed to individuals with active or a history of kidney stones (nephrolithiasis). Topiramate should also be avoided in pregnant women due to an increased risk of birth defects, especially cleft palate.
10. Melatonin
Melatonin is a hormone made by the pineal gland in the brain and helps control the sleep and wake cycle of humans. Small amounts of the hormone can be found in foods such as meats, grains, fruits, and vegetables. It’s commonly used as a supplement to promote restful sleep in individuals suffering from jet lag or sleep problems (insomnia). An Italian study published in Cephalgia reported remission of cluster headaches in 50-percent of patients receiving a 10-mg oral dose of melatonin nightly. In patients responding to treatment with melatonin, cluster headaches remitted until the medication was discontinued.
No significant adverse effects have been reported with the administration of melatonin. It may be most useful for prophylaxis of cluster headaches in individuals who cannot tolerate any of the other drugs used to prevent this condition.
 / Shutterstock.com
/ Shutterstock.com